In a groundbreaking editorial published on May 29, 2025, in the esteemed journal Aging (Volume 17, Issue 5), Editor-in-Chief Marco Demaria, affiliated with the European Research Institute for the Biology of Ageing (ERIBA), University Medical Center Groningen (UMCG), and the University of Groningen (RUG), puts forth a visionary call to transform modern healthcare. His argument centers on an urgent paradigm shift: moving from the reactive management of chronic diseases to proactive extension of healthspan by addressing the fundamental biology of aging itself. This transformative approach aims to revolutionize preventive medicine and offers a promising avenue to curb the escalating burden of multimorbidity in aging populations worldwide.
Today’s healthcare frameworks predominantly focus on treating individual diseases after they manifest clinically, often resulting in complex and costly interventions with limited efficacy, especially for elderly patients suffering from multiple chronic conditions. Demaria highlights the limitations inherent in this reactive model, emphasizing how the coexistence of diseases such as cancer, cardiovascular ailments, and type 2 diabetes shares interconnected aging pathways. This intricate biological overlap exacerbates treatment difficulties and overwhelms healthcare infrastructures globally. The editorial challenges this status quo by advocating for capturing and intervening at the root biological mechanisms that propel aging and its associated morbidities.
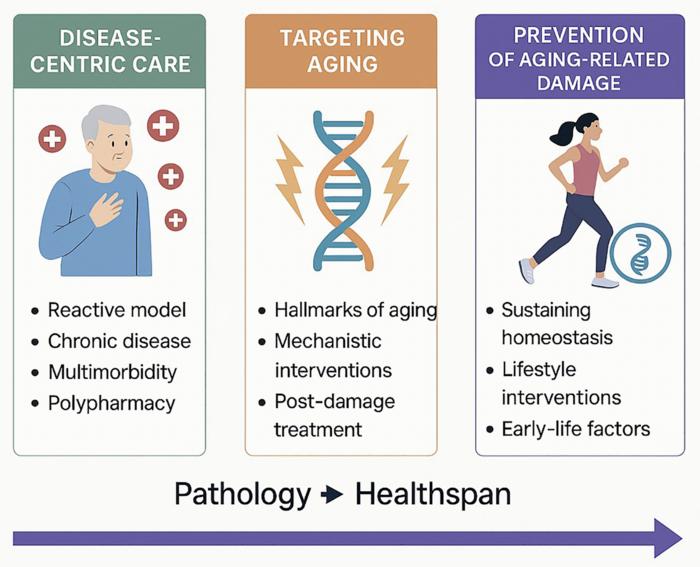
More specifically, Demaria delineates three distinct paradigms for healthcare management. The first is the conventional approach that remains strictly reactive—addressing disease symptoms post onset. The second paradigm represents an intermediate stage where emerging therapeutics target the biological damage that has already begun to accumulate with aging. This includes the use of senolytics, drugs designed to selectively eliminate senescent cells that accumulate and contribute to age-related tissue dysfunction, and rapalogs, which modulate pathways like mTOR to influence metabolic regulation and cellular aging. Lastly, the editorial champions the third, most progressive model: preventing aging-related molecular and cellular damage before it manifests. This life-course oriented strategy aspires not only to delay disease onset but to maintain biological homeostasis and restore resilience over a person’s lifespan.
Central to this proactive paradigm is the recognition that prevention must supersede treatment in importance. Lifestyle factors such as regular physical activity, balanced nutrition, adequate sleep, and stress management are underscored as critical modulators of aging pace and healthspan. Demaria further draws attention to the advent of biological age diagnostics, a cutting-edge toolset that leverages biomarkers, including epigenetic clocks and other omics-based metrics, to estimate an individual’s true physiological age beyond chronological years. This innovation enables personalized monitoring of aging trajectories and targeted interventions tailored to individual risk profiles, potentially revolutionizing how health preservation is approached on a population scale.
Equally significant is the focus on early-life determinants of aging and disease. Demaria advocates for optimizing maternal nutrition and healthcare during developmental windows, highlighting that life-course factors exert profound influences on aging biology. By instilling healthy physiological baselines from conception through childhood, the cumulative biological insults that precipitate age-related diseases later in life can be dramatically reduced. This holistic perspective aligns with growing evidence from longitudinal studies linking early-life environments to lifelong health outcomes and disease susceptibility.
Achieving this ambitious vision requires fundamental reforms in medical education and clinical training. Currently, the curricula for healthcare professionals seldom incorporate geroscience—the interdisciplinary study of aging mechanisms and their role in disease pathogenesis—nor do they emphasize healthspan extension strategies. Demaria insists that equipping future physicians and healthcare providers with geroscience expertise, alongside training in personalized preventive care, will be critical to successfully transitioning from disease-centric care to longevity-centered medicine. Such educational initiatives would redefine professional practice, empowering clinicians to become proactive facilitators of healthy aging rather than solely disease managers.
The editorial also stresses the necessity of fostering interdisciplinary collaboration among clinicians, biomedical researchers, data scientists, and policymakers to enable this new healthcare architecture. Integrating multi-omic data, including genomics, transcriptomics, proteomics, and metabolomics, is poised to enhance the precision and predictive power of aging diagnostics and interventions. Combined with real-world lifestyle data and longitudinal health tracking, this integrative approach can inform data-driven public health policies and resource allocation strategies that prioritize healthspan extension and reduce healthcare system strain.
Demaria’s vision also anticipates the socio-economic benefits of a healthspan-centered model. By focusing upstream on preventive interventions that decelerate biological aging, the incidence and severity of chronic age-related diseases can decline, translating to reduced healthcare expenditures and improved quality of life for aging individuals. Such systemic efficiencies would not only alleviate individual suffering but also enhance societal productivity and sustainability amidst rapidly aging demographics worldwide.
Technological advances in senolytic and rapalog therapeutics are particularly promising, offering mechanisms to selectively clear dysfunctional cells and recalibrate cellular metabolism, respectively. Early clinical trials suggest these interventions can attenuate or even reverse certain age-related phenotypes, supporting the editorial’s call to integrate geroprotective agents into routine clinical practice. Nevertheless, the broader adoption of these therapies demands rigorous long-term studies, regulatory approvals, and ethical considerations that account for complexities inherent in modulating fundamental aging processes.
In synthesizing these themes, Demaria’s editorial situates aging biology at the forefront of a healthcare revolution. He envisions a future where medicine transcends episodic treatment and embraces lifespan optimization with personalized, preventive, and predictive strategies firmly rooted in molecular geroscience. Importantly, adopting this third paradigm requires a cohesive societal shift, prioritizing research funding, policy-making, and healthcare delivery reforms to actualize the promise of healthier longevity.
Ultimately, this editorial resonates as a clarion call to rethink healthcare through a lens focused on the biological underpinnings of aging. By unraveling the molecular drivers of senescence, inflammation, and metabolic dysfunction, and marrying these insights with novel diagnostics and therapeutics, the path to extended healthspan and transformative healthcare systems becomes increasingly tangible. Dr. Marco Demaria’s vision challenges the global medical community to pivot swiftly and decisively toward a future where age-associated disease is not merely managed but fundamentally prevented.
Subject of Research: Not applicable
Article Title: Rethinking healthcare through aging biology
News Publication Date: 29-May-2025
Web References:
References: Not provided
Image Credits: Copyright © 2025 Demaria. Distributed under Creative Commons Attribution License (CC BY 4.0).
Keywords: healthcare, aging, senolytics, epigenetics, medical education