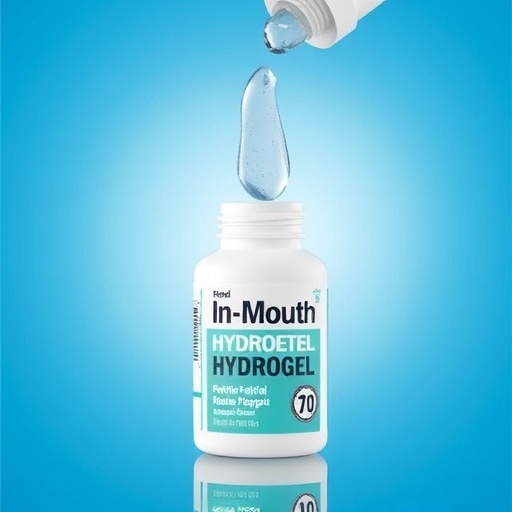
A groundbreaking advancement in the treatment of xerostomia, commonly known as dry mouth, has been unveiled by a team of researchers who engineered a novel polymer-based hydrogel capable of sustained artificial saliva release. This innovative biomaterial, designed to mimic the protective and lubricative functions of natural saliva, promises a transformative approach to a condition that affects millions worldwide, especially those undergoing intensive medical therapies that impair salivary gland function. By leveraging the unique properties of poly(hydroxyethyl methacrylate) (pHEMA), a polymer widely known for its biocompatibility and widespread use in medical devices, the scientists have crafted a saliva-gel reservoir that absorbs substantial quantities of artificial saliva and releases it gradually within the oral cavity.
Saliva performs an array of critical physiological roles. Beyond facilitating mastication and swallowing, it acts as a defensive barrier against microbial invasion and contributes enzymes essential for digestion. Conditions such as chemotherapy, radiation therapy, and hemodialysis are notorious for disrupting saliva production, resulting in discomfort, increased risk of oral infections, dental caries, and compromised quality of life. Conventional pharmacological treatments often focus on stimulating residual salivary gland activity or providing short-term relief, yet they fall short in addressing the chronic nature of xerostomia and are frequently accompanied by side effects including mucosal irritation and enamel degradation. This new hydrogel system aims to circumvent these limitations by serving as a reservoir that delivers artificial saliva directly and continuously.
Central to the hydrogel’s design is the integration of artificial saliva formulations within the matrix of pHEMA. Artificial saliva closely replicates the composition of natural saliva, primarily composed of water and mucins—gel-forming glycoproteins that imbue natural saliva with its lubricating and antimicrobial properties. The researchers achieved a stable mixture that can be implanted discreetly inside the oral cavity, for example under the tongue or along the inner cheek, without impeding normal oral functions or causing discomfort. Importantly, the hydrogel’s transparency and soft consistency render it practically unnoticeable, an essential feature for patient compliance.
The capacity of the hydrogel to store saliva was quantitatively assessed by submerging the polymer in artificial saliva for six hours, during which it expanded to approximately four times its original volume. This volumetric swelling is an indicator of the gel’s hydration capability and its potential to hold clinically relevant amounts of artificial saliva. Such a degree of absorption is remarkable given the hydrogel’s compact size, roughly comparable to a U.S. quarter, highlighting its feasibility for use in everyday settings without inconvenience.
Release kinetics of the saliva from the hydrogel were characterized at physiological temperature—98.6 degrees Fahrenheit (37 degrees Celsius)—to simulate the intraoral environment. The gel exhibited a biphasic release profile, emitting saliva rapidly in the initial phase before gradually tapering off over a four-hour period. This temperature-responsive behavior underscores a thermal trigger mechanism inherent to pHEMA, whereby molecular mobility increases with warmth, facilitating controlled diffusion of the hydration medium. The sustained release ensures prolonged moisturization, mitigating the persistent dryness that patients with xerostomia endure between doses of conventional treatments.
Reusability is another hallmark of this hydrogel system. Through five consecutive trials with the same reservoir, the release of artificial saliva remained consistent, indicating that the polymer network maintains structural integrity and functional stability over multiple use cycles. This attribute not only enhances patient convenience but also suggests potential economic benefits by reducing the frequency of replacement needed for oral care devices.
Biocompatibility assessments, pivotal for any implanted material, demonstrated that the hydrogel does not adversely affect cellular viability or proliferation when in contact with cultured oral cells. This facet confirms that the hydrogel is safe for persistent presence within the mouth, eliminating concerns about cytotoxic effects or provoking inflammatory responses that could exacerbate oral health complications.
Looking forward, the research team has expressed intentions to enhance the hydrogel’s mechanical resilience and optimize its saliva release capacity further. One promising avenue under exploration involves the incorporation of biodegradable components to make the implant fully dissolvable after its therapeutic lifespan, thus obviating the need for removal procedures and improving patient experience.
The implications of this technology extend beyond xerostomia management. Controlled release hydrogels such as this may be adapted to deliver various therapeutics in the oral cavity or other mucosal sites, opening avenues for localized treatment of diverse conditions ranging from oral infections to systemic diseases detectable through saliva biomarkers. The marriage of polymer science with biomedical engineering showcased here exemplifies the interdisciplinary innovation required to tackle complex health challenges.
Moreover, this hydrogel platform reflects a broader trend toward personalized and patient-friendly medical devices designed to integrate seamlessly into daily life without invasive interventions. For individuals debilitated by dry mouth, often a secondary effect of cancer therapies or chronic illnesses, this technology heralds hope for restored oral comfort and preserved oral health, significantly enhancing overall wellbeing.
With millions afflicted by xerostomia globally and existing treatments falling short, this new polymer-based saliva reservoir represents a vital step towards filling an urgent clinical need. The ongoing research efforts aimed at refining this approach and translating it into practical therapeutic options will be keenly watched by both the scientific community and clinicians focused on supportive care.
This innovative hydrogel system not only pushes the envelope of materials science but also epitomizes the potential of chemistry to directly improve patient outcomes. Through collaborative research and continued development, this saliva-gel holds promise to revolutionize how dry mouth is managed, alleviating a debilitating symptom and enriching patient quality of life worldwide.
Subject of Research: Development of a poly(hydroxyethyl methacrylate)-based hydrogel for sustained release of artificial saliva to treat xerostomia (dry mouth).
Article Title: “Poly(hydroxyethyl methacrylate) Saliva-Gel: A Polymer-Based Solution for Xerostomia Treatment”
News Publication Date: 17-Jul-2025
Web References: http://dx.doi.org/10.1021/acsapm.5c00881
References: Adapted from ACS Applied Polymer Materials 2025, DOI: 10.1021/acsapm.5c00881
Image Credits: Adapted from ACS Applied Polymer Materials 2025, DOI: 10.1021/acsapm.5c00881
Keywords
Chemistry, Health and medicine