In recent years, the intersection of psychological diagnosis and societal perceptions has come to the forefront, particularly when it comes to children facing disruptive behavior disorders. The study “Disruptive Behavior Disorders and Trauma in Children: Potential Implicit Biases in Diagnosis” by Bassford, Haberstroh, and Keene dives deep into the complexities of diagnosis processes that can disproportionately affect vulnerable populations, particularly children suffering from trauma. This exploration is not merely academic; it has profound implications for how these disorders are understood and treated across diverse contexts, raising questions about broader issues of equity in psychological care.
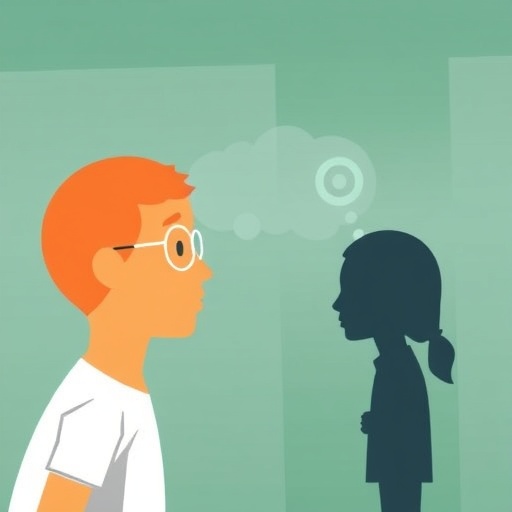
Disruptive behavior disorders, which include conditions such as Attention-Deficit/Hyperactivity Disorder (ADHD) and Oppositional Defiant Disorder (ODD), are often misdiagnosed or misunderstood, especially in children who have experienced trauma. The lens through which these disorders are viewed can significantly influence the diagnoses given by healthcare professionals. Implicit biases—those unconscious associations or attitudes—may lead practitioners to perceive the behavior of children from certain backgrounds differently than those from others. This can result in misdiagnosis, inadequate treatment, and ultimately, continued suffering for the child.
The research conducted by Bassford et al. sheds light on how these implicit biases manifest in clinical settings. By analyzing case studies and clinical outcomes, the authors provide a comprehensive look at how personal, social, and cultural factors intertwine in the diagnostic process. For instance, a child from a low-income household exhibiting disruptive behaviors may be labeled as defiant and problematic, while a child from a more affluent background displaying similar behaviors may be viewed through a lens of understanding that considers environmental factors. Thus, a child’s socio-economic context can inadvertently influence clinical judgments.
In addition to cultural and socioeconomic factors, the psychological implications of trauma cannot be overstated. Many children diagnosed with disruptive behavior disorders have histories laden with adverse childhood experiences (ACEs), such as neglect, abuse, or witnessing violence. These experiences can profoundly affect their behavior and emotional regulation. Yet, when clinicians fail to recognize the impact of trauma due to implicit biases, they may be inclined to attribute the child’s behavior solely to the disorder, ignoring the underlying trauma. The result is a failed opportunity for appropriate interventions that address the root causes of behavior, perpetuating a cycle of misunderstanding and mistreatment.
Addressing these biases requires a concerted effort at multiple levels, as proposed by the authors. Training programs for healthcare professionals must emphasize cultural competence and sensitivity when diagnosing disruptive behavior disorders. By understanding that a child’s behavior is not solely a reflection of their disorder but may be rooted in their lived experiences, clinicians can shift their approach to diagnosis and treatment. This paradigm shift could lead to a more nuanced understanding of disruptive behaviors as complex reactions to stressors and traumas.
The implications of effectively addressing these implicit biases are far-reaching. By improving diagnostic accuracy and ensuring that children receive appropriate support, we can shape a path toward healthier outcomes. Psychological health professionals equipped with a robust understanding of these biases will be better prepared to recommend therapeutic approaches that focus on healing trauma rather than merely managing disruptive behaviors. These could include trauma-informed care techniques that recognize the pain and challenges faced by these children.
Moreover, the study’s findings call for the involvement of policymakers and educational institutions in furthering awareness and training in this area. Schools, often on the front lines of identifying and addressing behavioral issues, should be equipped to understand the broader context of a child’s behaviors. Initiatives at the school level might combine educational programs for teachers on recognizing signs of trauma with counseling resources that can facilitate early intervention.
The research also highlights the necessity for a shift in societal attitudes towards children with disruptive behavior disorders. Stigma surrounding mental health can create barriers to treatment and may influence the ways children are perceived within their communities. Schools and families should work together to foster an environment that encourages open discussions about mental health, ensuring that children feel supported rather than isolated by their challenges.
Ultimately, the findings from Bassford et al. suggest that the future of treating disruptive behavior disorders in children lies in a holistic understanding of each child’s unique circumstances. By confronting implicit biases and acknowledging the trauma that often underpins these behaviors, we can better serve vulnerable populations. Creating systems that recognize and respond to the complexities of each child’s experiences is crucial for fostering emotional wellbeing and resilience.
In conclusion, the dialogue initiated by this study is critical for the ongoing evolution of mental health practices. Advocating for awareness around implicit biases can catalyze change within clinical settings, fostering a more equitable and effective approach to diagnosis and treatment of disruptive behavior disorders. By prioritizing trauma-informed and culturally competent care, the mental health community can work toward ensuring that every child receives the support they need to thrive.
This multifaceted approach to understanding and addressing the challenges of disruptive behavior disorders not only benefits individual children but can ultimately lead to healthier families and communities. Through awareness, education, and commitment to equity, we can build a more just system that responds compassionately and effectively to the needs of every child.
Subject of Research: Implicit biases in the diagnosis of disruptive behavior disorders in children and their connection to trauma.
Article Title: Disruptive Behavior Disorders and Trauma in Children: Potential Implicit Biases in Diagnosis?
Article References:
Bassford, J.H., Haberstroh, S. & Keene, C.N. Disruptive Behavior Disorders and Trauma in Children: Potential Implicit Biases in Diagnosis?.
Journ Child Adol Trauma (2025). https://doi.org/10.1007/s40653-025-00784-0
Image Credits: AI Generated
DOI:
Keywords: disruptive behavior disorders, trauma, implicit bias, diagnosis, children, mental health, cultural competence, education.