In a groundbreaking study led by van der Heijden and colleagues, the intricate landscape of plasma proteomics has been explored in relation to two critical clinical conditions: septic shock and alcohol-related pancreatitis. This research is pivotal because these conditions not only present significant challenges in therapeutic management but also share underlying pathological mechanisms that demand comprehensive understanding. By employing a hyaluronan-centered approach, the authors have peeled back layers of complexity, revealing promising avenues for diagnosis and treatment.
Septic shock is characterized by a profound dysregulation of the immune response to infection, leading to systemic inflammation and multi-organ failure. The study emphasizes the need for precision medicine in managing septic shock, highlighting the role that plasma proteins play in the inflammatory cascade. Proteomics, the large-scale study of proteins, allows researchers to identify biomarkers that can predict disease outcomes, tailor treatment strategies, and ultimately improve patient survival rates.
On the other hand, alcohol-related pancreatitis brings a different layer of complexity. This condition often results from chronic alcohol consumption, which induces inflammation of the pancreas and presents with symptoms ranging from mild abdominal pain to severe systemic complications. The metabolomic adjustments and ensuing proteomic alterations are key to understanding not only the extent of pancreatic injury but also the body’s response to such insult. By juxtaposing these two conditions, the researchers aim to delineate common pathways that might be exploited for therapeutic gain.
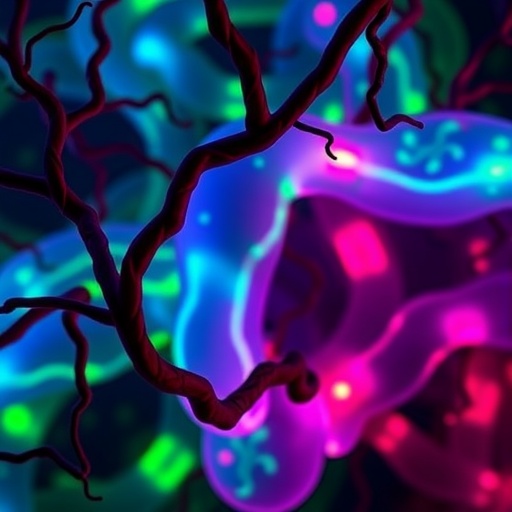
Hyaluronan, a glycosaminoglycan present in the extracellular matrix, emerged as a central theme in the study. As a component involved in inflammation and tissue repair, hyaluronan’s levels can significantly fluctuate during pathological processes such as septic shock and pancreatitis. This study meticulously examines how plasma concentrations of hyaluronan correlate with disease severity, offering insights into its potential utility as a biomarker for monitoring these conditions. By focusing on this molecule, the researchers underscore its dual role as both a participant in disease progression and a potential therapeutic target.
The methodological rigor of this study deserves special mention. The researchers employed sophisticated mass spectrometry techniques to analyze plasma samples from patients afflicted with septic shock and alcohol-related pancreatitis. This approach not only allowed for a detailed characterization of protein expressions but also afforded a high level of sensitivity and specificity. Such precision is vital in capturing the dynamic changes in plasma proteomes that can emerge even in the early stages of disease progression.
Moreover, the research highlights the limitations of current diagnostic practices in these acute conditions. Traditional markers do not sufficiently discriminate the severity of septic shock nor do they efficiently predict the course of alcohol-related pancreatitis. As such, the identification of new biomarkers, especially those grounded in proteomic data, could herald a new era of diagnostic capabilities that enhance clinical decision-making and patient care.
The implications of these findings extend beyond the confines of academic research. In clinical settings, a deeper understanding of the proteomic profiles associated with septic shock and alcohol-related pancreatitis could influence therapeutic approaches. Tailored therapeutic interventions that consider the unique proteomic landscape of individual patients could be developed. For instance, patients exhibiting specific proteomic signatures that correspond to heightened inflammatory responses may benefit from targeted anti-inflammatory therapies, thus enhancing treatment efficacy.
Furthermore, the collaborative nature of this research speaks volumes about the interdisciplinary approaches required to tackle complex medical challenges. Collaboration among clinicians, biochemists, and bioinformaticians has resulted in a rich dataset that not only builds upon existing knowledge but also opens up avenues for future investigations. The study sets a precedent for future research initiatives to adopt similar collaborative strategies in probing other complex medical conditions.
Looking ahead, it will be crucial for future studies to validate the findings of this research in larger, diverse populations. Replicating the study across different demographics will ensure that the identified biomarkers are robust and generalizable. Moreover, as the field of proteomics continues to evolve, advancements in technology and methodology will undoubtedly enhance the resolution of biomarker identification. This will in turn support the clinical application of findings derived from proteomic analyses.
In conclusion, the pioneering study spearheaded by van der Heijden and colleagues signifies a substantial advancement in our understanding of septic shock and alcohol-related pancreatitis at the proteomic level. By focusing on hyaluronan and other plasma proteins, the researchers not only elucidate shared pathophysiological mechanisms but also chart a path toward improved diagnostic and therapeutic options. As the medical community digests these findings, there lies great hope that such insights will translate into tangible improvements in patient outcomes across the globe.
The study serves as a call to action for the ongoing exploration of proteomics in the realm of critical care medicine. Given the dynamic nature of human disease, continuous examination and hypothesis testing will ensure that researchers and clinicians can adapt to emerging challenges. The promise of more effective interventions that stem from a deeper understanding of plasma proteins emphasizes the importance of this avenue of research in the ever-evolving landscape of medicine.
The need for interdisciplinary collaboration, rigorous methodologies, and the exploration of novel biomarkers remains paramount as we strive to transform our understanding of complex conditions like septic shock and alcohol-related pancreatitis. This research not only tells a compelling story of scientific inquiry but also lays the groundwork for future innovations that may fundamentally change how these life-threatening conditions are managed and treated.
Through the lens of this study, we are reminded of the delicate dance between inflammation and healing, and how decoupling the former through precise clinical interventions can lead to better outcomes for the latter. The journey of discovery continues, and with it, the potential to save countless lives that hang in the balance.
Subject of Research: Plasma proteomics in septic shock and alcohol-related pancreatitis
Article Title: Plasma proteomics in septic shock and alcohol-related pancreatitis: a hyaluronan-centered approach.
Article References: van der Heijden, J., Mazubane, A., Sallisalmi, M. et al. Plasma proteomics in septic shock and alcohol-related pancreatitis: a hyaluronan-centered approach. Clin Proteom 22, 31 (2025). https://doi.org/10.1186/s12014-025-09556-2
Image Credits: AI Generated
DOI:
Keywords: Plasma proteomics, Septic shock, Alcohol-related pancreatitis, Hyaluronan, Biomarkers, Mass spectrometry, Inflammation, Critical care medicine.