In the relentless quest to enhance outcomes for extremely premature infants, a pioneering medical innovation known as the Artificial Amnion and Placenta Technology (AAPT) is poised to revolutionize neonatal care. This groundbreaking technology is designed to replicate key functions of the natural amniotic sac and placenta, offering a life-sustaining environment outside the womb for the tiniest and most vulnerable humans. As first in-human trials of AAPT approach realization, healthcare experts worldwide are gearing up not only for the technical challenges but also for the profound ethical and legal considerations that accompany such a transformative step.
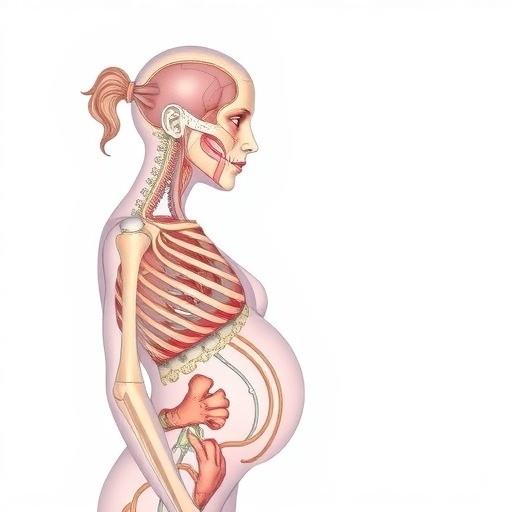
AAPT represents the zenith of bioengineering and neonatology convergence, providing an artificial womb environment that supports critical physiological processes usually maintained by the maternal body. At its core, the system mimics the amniotic sac’s protective, fluid-filled milieu while simultaneously replicating placental functions such as gas exchange, nutrient delivery, and waste removal. This intricate balance is critical because extremely premature infants, those born before 28 weeks of gestation, face devastating mortality and morbidity rates under existing neonatal intensive care protocols. The promise of AAPT lies in its ability to bridge this gap and mitigate the lifelong disabilities often resulting from premature birth.
The path toward human clinical trials, however, requires more than just technological sophistication. The intricate interface between cutting-edge science and human values necessitates comprehensive empirical research involving key stakeholders, including healthcare professionals, ethicists, and, critically, prospective parents. A recent study led by de Boer and colleagues (2025) focuses on the thorny issues surrounding counseling and informed consent in the context of AAPT trials, bringing to light the myriad considerations that must be reconciled to proceed responsibly.
The ethical imperatives for counseling prospective parents considering enrolling their extremely premature infants in AAPT trials are multifaceted. Parents facing imminent premature delivery often navigate overwhelming emotional stresses intertwined with complex medical information. Providing clear, balanced, and empathetic counseling is paramount to facilitating genuinely informed decisions. This involves not only explaining the scientific nuances of AAPT but also candidly addressing the uncertainties, potential risks, and long-term unknowns inherent in any first-in-human trial.
Legal frameworks governing clinical trials add yet another layer of complexity. The novelty of AAPT means existing regulations may not comprehensively capture the unique risks and benefits inherent in maintaining life via an artificial placenta system. Informed consent protocols must be rigorously evaluated and possibly adapted to ensure comprehension and voluntariness, especially given the severely time-pressured context of premature labor. The study underscores the necessity of multidisciplinary collaboration to develop consent processes that respect parental autonomy while prioritizing infant welfare and scientific integrity.
From a technical standpoint, AAPT’s design involves microfluidic oxygenators, biocompatible membranes, and highly controlled temperature and pressure conditions to emulate womb-like conditions precisely. The infant is supported in a fluid-filled chamber, maintaining a sterile, thermoregulated environment that minimizes physical trauma and infection risk. The system’s interface with the neonatal circulatory system allows for extracorporeal oxygen and nutrient delivery tailored to the infant’s physiological demands, maintaining vital parameters within safe limits.
This delicate balancing act is challenged by developmental considerations unique to the fetal physiology. For example, the pulmonary circulation of a fetus bypasses the lungs via the ductus arteriosus; thus, the artificial placenta must replicate the oxygen transfer role typically performed by the maternal lungs without triggering untimely circulatory adaptations. Moreover, incorporating feedback mechanisms responsive to dynamic changes in the infant’s condition demands sophisticated sensor integration and automation within the device.
The societal implications of AAPT extend beyond immediate clinical application. Should this technology prove safe and efficacious, it could redefine viability thresholds and reshape ethical debates around abortion, neonatal care, and reproductive rights. The prospect of gestating a fetus entirely outside the human body challenges deeply held notions of parenting, gestation, and human development. Hence, the responsibility borne by researchers and clinicians extends into the broader cultural and philosophical domains.
In-depth empirical research carried out by de Boer and colleagues interrogates parental and healthcare professional perspectives on the acceptability and understanding of counseling and consent processes for AAPT. Their findings illuminate divergences and convergences in expectations, highlighting the critical role of trust and transparent communication in fostering informed participation. Importantly, the research advocates for tailored counseling approaches that accommodate diverse cultural, social, and educational backgrounds to avoid exacerbating health disparities.
The urgency of preparing ethically sound clinical trial frameworks is accentuated by the precarious prognosis facing extremely premature infants with current standard care. Neonatal intensive care units globally report survival rates plummeting under certain gestational ages, coupled with high incidence of neurodevelopmental impairments, respiratory complications, and sensory deficits. AAPT strives not merely to extend survival but to enhance quality of life, necessitating outcome measures that encompass long-term developmental trajectories, not just immediate physiological stabilization.
Navigating the legal waters surrounding AAPT trials involves harmonizing international regulations with evolving ethical guidelines. Regulatory bodies must grapple with defining the infant’s legal status during artificial gestation – is this a patient, a research subject, or a partially developed neonate? Consent guardianship, liability in the event of adverse outcomes, and guidelines for data privacy all require meticulous clarification. The involvement of bioethicists, lawyers, neonatologists, and patient advocacy groups is indispensable in crafting these frameworks.
Technological challenges remain formidable. Ensuring the artificial environment’s sterility, preventing immunological reactions to extracorporeal circulation, and fine-tuning nutrient formulations to mimic placental transfer are areas of ongoing research. Additionally, scaling the technology for broader clinical use demands cost-effective manufacturing and rigorous quality control measures, balancing innovation with accessibility to prevent inequities in neonatal care availability.
Crucially, the first in-human trials represent a milestone in translational medicine, marking the transition from promising animal studies to direct human application. This step must be marked by cautious optimism, robust monitoring protocols, and adaptive trial designs capable of responding to unforeseen complications. Real-time data collection and the establishment of international registries can provide invaluable insight into AAPT’s performance and safety profiles.
Public engagement and education emerge as vital components in the rollout of AAPT. Raising awareness about the technology’s potential and limitations can help temper unrealistic expectations and foster informed public discourse. Media portrayal, ethical debates, and stakeholder feedback loops should be managed with care to maintain social trust and facilitate the ethical integration of artificial gestation into clinical practice.
As science propels forward, the Artificial Amnion and Placenta Technology encapsulates the dual marvel and responsibility inherent in medical innovation. It offers hope for countless infants on the threshold of survival while demanding scrupulous attention to the human dimensions of care and consent. The evolving dialogue shaped by empirical studies like de Boer et al.’s will be instrumental in steering this extraordinary endeavor toward outcomes that honor both technological brilliance and the sanctity of human life.
—
Subject of Research: Counseling and informed consent challenges in first in-human trials of Artificial Amnion and Placenta Technology (AAPT) for extremely premature infants.
Article Title: Human artificial placenta technology-trials: counselling and informed consent using healthcare professionals’ and parental perspectives.
Article References:
de Boer, A., Krom, A., Kalaai, R. et al. Human artificial placenta technology-trials: counselling and informed consent using healthcare professionals’ and parental perspectives. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04051-8
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41390-025-04051-8