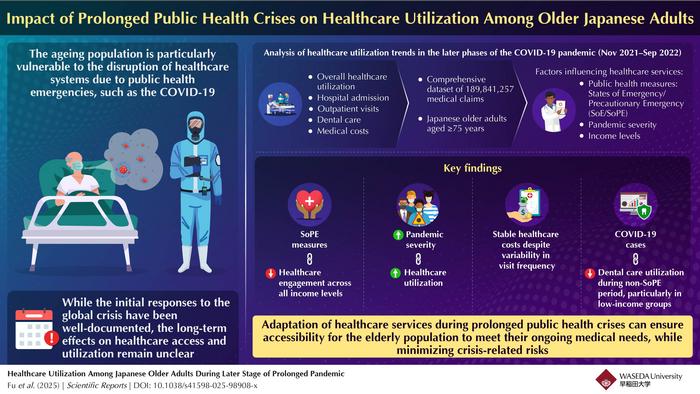
As the world continues to grapple with the multifaceted consequences of the COVID-19 pandemic, a particularly vulnerable group has remained at the forefront of concern: the elderly. A new comprehensive study conducted by researchers at Waseda University, Japan, sheds light on the subtle yet significant shifts in healthcare utilization among adults aged 75 and above during the latter stages of the prolonged COVID-19 pandemic. This research provides critical insights into how healthcare systems can adapt to maintain service delivery amid ongoing public health crises, ensuring that the most susceptible populations are not left behind.
The onset of the COVID-19 pandemic in late 2019 triggered an unprecedented global health emergency. Governments worldwide implemented stringent public health measures including social distancing, mandatory mask-wearing, and declarations of states of emergency to curb viral transmission. While these interventions were vital to controlling the spread, they also inadvertently disrupted routine healthcare services, particularly for older individuals who face heightened risks from both the virus and the interruption of ongoing medical care. Initial investigations explored the immediate impact of the pandemic, but the extended phases—with their evolving viral variants, relaxing restrictions, and growing vaccination coverage—remained less understood, especially from a healthcare utilization perspective in the elderly.
To bridge this critical knowledge gap, the Waseda University research team embarked on an observational study focusing on Japan’s aged population, one of the oldest in the world, supported by a universal healthcare infrastructure. The study period spanned from November 2021 to September 2022, encapsulating a phase in which newer SARS-CoV-2 variants exhibited reduced virulence, and societal controls gradually eased. By meticulously analyzing an extraordinarily large dataset comprising nearly 190 million medical claims linked to income tax records, the research team was able to correlate healthcare usage trends with socioeconomic status, geographic variables, and the timing of public health interventions.
One of the pivotal findings of this extensive analysis was the identification of a modest decline in patient visits and outpatient consultations correlating with the imposition of precautionary measures. Despite this decrease in the frequency of visits, total healthcare expenditures and overall service utilization remained remarkably stable. This pattern suggests that while older adults may have postponed or spaced out visits, healthcare providers adapted their delivery models to sustain the intensity of care, minimizing potential deterioration in patient outcomes amid the crisis.
Further dissecting the data revealed geographic disparities tied to crisis intensity and policy enforcement. Regions experiencing more severe COVID-19 outbreaks and stricter public health mandates saw more pronounced decreases in healthcare access. However, these fluctuations did not universally translate into reduced service intake, hinting at adaptive healthcare delivery models such as telemedicine or mobile medical units responding to localized needs. Most notably, the study’s socioeconomic analysis uncovered a critical exception within dental care: lower-income older adults exhibited significantly fewer dental visits compared to their higher-income counterparts, signaling emerging inequalities exacerbated by the pandemic context.
The implications of fluctuating dental care utilization among socioeconomically disadvantaged elderly groups extend beyond immediate oral health repercussions. Dental conditions have documented associations with systemic diseases such as cardiovascular disorders and diabetes, making sustained access to preventive and curative dental services vital for comprehensive elder care. The study’s authors assert that such disparities emphasize the need for integrated healthcare strategies explicitly designed to bridge gaps in dental and other preventive services during public health emergencies.
Drawing from their findings, the research team posits that healthcare systems must incorporate multifaceted adaptations to ensure resilient access for aging populations during crises. Suggested measures include the implementation of integrated monitoring systems capable of real-time healthcare utilization tracking, strengthening safety protocols to safeguard patients and healthcare workers alike, and deploying early warning mechanisms to anticipate service disruptions. Additionally, introducing flexible care delivery modalities, such as remote consultations and mobile clinics, can significantly alleviate access barriers for vulnerable groups confined by mobility restrictions or infection fears.
Associate Professor Rong Fu, lead author of the study, underscores the broader public health significance of these insights: “Our research highlights the necessity for health policymakers to design nuanced, adaptive interventions that preserve equitable healthcare access during prolonged crises. Maintaining service intensity, even when traditional visit frequencies wane, is paramount to protecting vulnerable elderly populations from adverse health outcomes.” This statement reflects a paradigm shift from reactive emergency responses toward proactive system resilience and equity-oriented healthcare planning.
From a methodological perspective, the study’s use of an exceptionally large, linked dataset from Japan’s universal healthcare and tax systems lends robustness to its conclusions. By combining claims data with socioeconomic indicators, the researchers could delineate nuanced utilization patterns beyond simple visit counts, capturing service intensity and expenditure trends. This analytical depth enables a comprehensive understanding of how various factors—ranging from policy enforcement and regional COVID-19 burden to income disparities—intersect to shape healthcare behaviors among older adults.
The timing of the research, capturing the transitional phase of the pandemic marked by a shift to less virulent viral variants and pandemic fatigue in public behaviors, offers valuable lessons for future outbreaks. It points to the importance of sustained vigilance and adaptive service models even when disease severity lessens, as disruptions in care can persist and exert long-term health consequences. The findings also highlight how universal healthcare systems, when coupled with targeted adaptations, can moderate disparities and maintain service continuity during systemic shocks.
Importantly, this study serves as a clarion call for integrating socioeconomic assessments into emergency healthcare planning. The evident disparity in dental care access among lower-income elderly patients is a potent reminder that crises do not impact populations uniformly. Tailored interventions targeting at-risk groups, including subsidies, mobile service delivery, and community outreach programs, could mitigate widening health inequities amplified by pandemic-induced disruptions.
Looking forward, the research team advocates for continued research into healthcare utilization across diverse populations and healthcare sectors during prolonged emergencies. Expanding biomonitoring and patient-centered data collection coupled with advanced analytics may enable real-time adjustments to healthcare delivery strategies, minimizing adverse outcomes and optimizing resource allocation. Incorporating behavioral health dimensions, such as fear of infection and pandemic-related anxiety, could further refine understanding of healthcare avoidance behaviors observed in this and other studies.
In conclusion, the Waseda University study illuminates critical dynamics of healthcare utilization among elderly populations in prolonged pandemic settings. It highlights the resilience and adaptability of healthcare systems but also warns of persistent gaps, particularly socioeconomic disparities that warrant focused policy action. As the global community prepares for future health emergencies, these insights inform the design of more equitable, flexible, and robust healthcare frameworks that safeguard vulnerable populations’ access to essential services without compromising infection control imperatives.
Subject of Research: People
Article Title: Healthcare utilization among Japanese older adults during later stage of prolonged pandemic
News Publication Date: 22-Apr-2025
Web References: https://doi.org/10.1038/s41598-025-98908-x
References:
Fu, R., Liu, S., Oikawa, M., Noguchi, H., & Kawamura, A. (2025). Healthcare utilization among Japanese older adults during later stage of prolonged pandemic. Scientific Reports. https://doi.org/10.1038/s41598-025-98908-x
Image Credits: Rong Fu from the Faculty of Commerce, Waseda University, Japan
Keywords: COVID-19 pandemic, healthcare utilization, elderly population, Japan, health disparities, dental care, public health emergencies, healthcare adaptation, universal healthcare, socioeconomic status