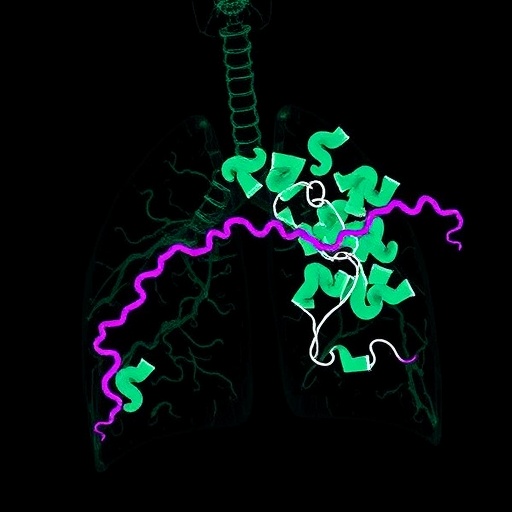
Recent developments in cancer research have illuminated crucial insights into the mechanisms that render lung adenocarcinomas resistant to immunotherapy. A study led by Parker, R.E. and colleagues has revealed that high levels of the protein PER1 are closely associated with mutations in the STK11 gene—a common occurrence in lung adenocarcinoma. This correlation not only underscores the vital relationship between molecular alterations and immunotherapy effectiveness but also proposes a potential pathway for targeted therapeutic strategies.
In the field of oncology, understanding the genetic factors that contribute to cancer progression is paramount. The findings of this study highlight how PER1, a known regulator of circadian rhythms, may also play a pivotal role in tumor biology. Researchers have long been exploring the ways in which circadian genes influence various physiological processes, including cell proliferation and apoptosis, suggesting that the intricate relationship between time and biological mechanisms could provide valuable therapeutic targets.
The mutation of STK11, also known as LKB1, is frequently observed in lung adenocarcinomas, and its implications for tumor growth and response to treatment have been extensively studied. The presence of STK11 mutations has been linked to a more aggressive disease phenotype and has been consistently associated with poor responses to immunotherapies, particularly those targeting immune checkpoint pathways. The study in question reinforces this notion by demonstrating that elevated PER1 levels may signal a critical intersection between STK11 status and immunotherapy resistance.
One of the primary objectives of this investigation was to unravel the potential mechanisms underlying the association between PER1 expression and STK11 mutations. Researchers employed a multifaceted approach, integrating computational biology with experimental validation. By analyzing datasets that include genomic, transcriptomic, and clinical data, they established a robust framework for understanding how these molecules interact within the tumor microenvironment.
The notion that PER1 could serve as a biomarker for predicting immunotherapy outcomes is particularly exciting. Current therapies often grapple with the challenge of identifying patients who will benefit from treatment, and the identification of PER1 as a significant player offers a promising avenue for refining patient selection. By stratifying patients based on perioperative PER1 levels, clinicians may be able to enhance the efficacy of treatment regimens.
These findings also underscore the necessity for further research into the therapeutic implications of PER1 manipulation. The potential to modulate PER1 expression in lung adenocarcinoma could open new avenues for treatment strategies. Whether through pharmacological interventions or gene editing, harnessing the power of this circadian-related protein to improve patient outcomes is an objective that warrants serious attention from the medical research community.
In exploring the specific mechanisms by which PER1 influences immunotherapy response, the study provides a foundation for future investigations. Understanding whether PER1 directly influences the immune landscape of tumors or whether it participates in regulatory networks will be critical for the development of new therapeutic strategies. This points to the broader importance of dissecting the immunomodulatory roles of circadian genes.
Furthermore, the study emphasizes the significance of combinatorial approaches in cancer treatment. Given the complexity of the tumor microenvironment and the multitude of pathways involved in cancer progression, a more integrated understanding of molecular networks will be essential. Combining PER1 status with other biomarkers of immune response could lead to the creation of more nuanced and effective treatment plans tailored to individual patients.
The implications of this research extend beyond just lung cancer. As our understanding of the immune system and cancer continues to evolve, the role of circadian rhythms and their associated proteins could be universally relevant across various cancer types. This opens a door for cross-disciplinary research that bridges oncology, chronobiology, and immunology.
As researchers continue to delve deeper into the relationship between circadian biology and cancer, they may uncover additional layers of complexity. The interplay between time-of-day effects on drug metabolism, immune function, and tumor behavior presents an intriguing frontier. Innovations in this realm could eventually inform not only lung cancer treatment but also approaches to enhance overall cancer therapy efficacy across diverse malignancies.
Moreover, as we forge ahead in the era of personalized medicine, delineating the genetic signatures characteristic of diverse tumor types will allow clinicians to tailor interventions at an unprecedented level. The findings from Parker et al. serve as a striking reminder of the dynamic nature of cancer research, highlighting the importance of adapting our strategies in response to emerging evidence.
Collaborative efforts among researchers, clinicians, and biotechnology firms will be vital in translating these findings into clinical practice. Multidisciplinary teams equipped with a comprehensive understanding of biomolecular interactions can facilitate the development of innovative therapies that extend beyond traditional models. The promise of advancing our understanding of PER1 and STK11 mutations can set the precedent for future breakthroughs in the field.
In conclusion, the research conducted by Parker and his team offers a promising outlook on addressing a significant challenge in lung cancer management. By associating high PER1 expression with STK11 mutations and immunotherapy resistance, they have provided valuable insights into the underlying mechanisms that influence treatment efficacy. As the landscape of cancer treatment evolves, studies like this will undoubtedly serve as critical stepping stones toward more precise, effective, and personalized therapeutic strategies for patients battling lung adenocarcinoma and beyond.
Subject of Research: Role of PER1 and STK11 in lung adenocarcinoma and resistance to immunotherapy
Article Title: High PER1 expression is associated with STK11 mutation and clinical biomarkers of immunotherapy resistance in lung adenocarcinoma
Article References:
Parker, R.E., McSwain, L., Zhou, W. et al. High PER1 expression is associated with STK11 mutation and clinical biomarkers of immunotherapy resistance in lung adenocarcinoma.
J Cancer Res Clin Oncol 151, 223 (2025). https://doi.org/10.1007/s00432-025-06269-9
Image Credits: AI Generated
DOI: 10.1007/s00432-025-06269-9
Keywords: PER1, STK11, lung adenocarcinoma, immunotherapy resistance, biomarkers, cancer research, circadian rhythms