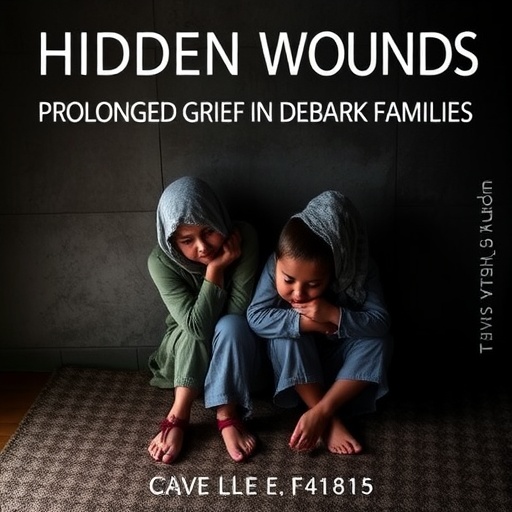
In the often-overlooked corners of global conflict zones, the emotional toll on the families of fallen soldiers remains a largely invisible crisis. A recent study conducted in Debark Town, North Ethiopia, sheds critical light on this phenomenon, revealing the profound psychological impact that prolonged grief exerts on families left behind. Published in BMC Psychology, the research by Ayalew, Yeniakal, and Tessema meticulously documents the lingering scars experienced by relatives of soldiers, illustrating how prolonged grief disorder (PGD) manifests within this community and disrupts the social and emotional fabric of their lives.
Prolonged grief disorder, distinct from typical bereavement, represents a persistent, intense yearning and preoccupation with the deceased that severely interferes with an individual’s daily functioning. The study focuses on families in Debark Town, where decades of political instability and armed conflict have resulted in high casualty rates. The authors detail how these families suffer enduring psychological wounds that are exacerbated by inadequate mental health resources and societal stigma surrounding grief. This research underscores the urgent need for culturally sensitive mental health interventions tailored to the war-affected populations.
The study deploys a mixed-methods approach, combining quantitative psychological assessments with qualitative interviews to capture the complexity of grief experiences among affected families. Standardized scales measuring symptoms of prolonged grief were employed alongside narrative analyses of personal testimonies. This dual approach elucidated not only the prevalence of PGD but also its multifaceted expressions—intrapersonal anguish, disrupted family dynamics, and community isolation. It reveals how grief in these settings is compounded by economic hardship and the absence of traditional mourning practices disrupted by conflict.
Scientific inquiry into grief has increasingly recognized prolonged grief disorder as a pathology requiring targeted intervention. In conflict zones such as Debark, however, limited infrastructure and cultural factors make diagnosis and treatment challenging. The authors highlight the significant gap between the mental health needs of bereaved families and the existing health services’ capacity. They advocate for the integration of grief counseling into primary health care and the training of local healthcare workers to recognize and address prolonged grief symptoms effectively.
The neurological underpinnings of prolonged grief disorder are elaborated upon through reference to current psychiatric literature. Changes in brain regions implicated in reward processing and emotional regulation—such as the anterior cingulate cortex and the amygdala—are discussed as biological correlates of entrenched sorrow. The study situates these findings within the context of prolonged exposure to trauma and loss, thereby framing prolonged grief as not solely an emotional response but also a neurobiological condition deserving comprehensive clinical attention.
In addition to clinical insights, the study emphasizes the social dimensions of prolonged grief. Families of fallen soldiers in Debark experience not only private suffering but public marginalization. Bereaved individuals are often excluded from community support networks, which exacerbates feelings of loneliness. This social isolation contributes to the severity and longevity of grief symptoms, forming a vicious cycle that hinders recovery. The article makes a compelling case for community-based interventions that rebuild social cohesion and foster collective healing.
The economic consequences of prolonged grief among these families are also examined. Loss of a breadwinner dramatically destabilizes family income, increasing vulnerability to poverty and food insecurity. The psychological distress linked to prolonged grief can impair the surviving relatives’ capacity to engage in productive employment or education, perpetuating socioeconomic disadvantage. By quantifying these impacts, the study situates prolonged grief not merely as a mental health issue but as a broader societal challenge with ramifications for economic development and stability.
The researchers draw attention to gendered aspects of prolonged grief, noting that women, particularly widows and mothers, often bear a disproportionate burden. Cultural expectations around mourning and caregiving roles intensify their psychological strain. Many female relatives report feeling trapped between personal grief and social pressures to maintain family cohesion. This gender-sensitive perspective enriches the understanding of how prolonged grief disorder unfolds differently across demographic groups within affected communities.
The methodological rigor of the study is underscored by its community-based participatory research framework. Local stakeholders were engaged throughout the research process to ensure cultural validity and ethical sensitivity. This collaboration not only facilitated accurate data collection but also empowered community voices in addressing mental health stigma. The participatory approach models a replicable framework for conducting mental health research in other conflict-affected, resource-limited regions.
Importantly, the study’s findings have implications beyond Ethiopia’s borders. Prolonged grief disorder among families of soldiers is an underreported global phenomenon in many contemporary conflict zones. Insights gathered from Debark Town can inform international humanitarian policies and mental health programming aimed at post-conflict recovery. By contextualizing prolonged grief within the broader matrix of trauma and displacement, the study advocates for integrated care models that address both psychological sequelae and social determinants of health.
The article’s discussion highlights promising avenues for therapeutic intervention. Evidence-based treatments such as complicated grief therapy (CGT) and cognitive-behavioral approaches are explored, with an emphasis on adapting these modalities to local cultural contexts. The authors suggest that incorporating traditional mourning rituals and community support structures into treatment protocols could enhance efficacy and acceptance. This synergy between modern psychiatry and indigenous practices provides a blueprint for culturally competent mental health care.
Another critical dimension analyzed is the impact of prolonged grief on the younger generation within these families. Children and adolescents who lose a parent to conflict are at elevated risk for a range of psychological and behavioral problems. The study calls for inclusive family-centered interventions that address intergenerational trauma and prevent the transmission of grief-related dysfunction. Early psychosocial support is positioned as essential to breaking cycles of mental ill-health perpetuated by unresolved mourning.
Technology’s role in expanding access to mental health care is briefly examined, with the authors advocating for mobile health (mHealth) platforms as potential tools in remote and underserved regions like Debark. Given widespread mobile phone usage, digital interventions could offer scalable solutions for grief counseling and psychoeducation. The incorporation of telepsychiatry and culturally tailored digital resources aligns with global trends toward democratizing mental health services.
Finally, the research serves as a poignant reminder that the human costs of war extend far beyond the battlefield. The invisible wounds of prolonged grief carve deep and lasting marks on the fabric of communities who have sacrificed loved ones in conflict. This comprehensive study from Debark Town not only advances scientific understanding of grief pathology but also calls for compassionate, multifaceted responses to support families in their long journey toward healing.
Subject of Research:
Prolonged grief disorder among families of soldiers in Debark Town, North Ethiopia
Article Title:
The unseen scars: prolonged grief among families of soldiers in Debark Town, North Ethiopia
Article References:
Ayalew, W.Z., Yeniakal, H.G. & Tessema, M.G. The unseen scars: prolonged grief among families of soldiers in Debark Town, North Ethiopia. BMC Psychol 13, 1275 (2025). https://doi.org/10.1186/s40359-025-03563-6
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s40359-025-03563-6