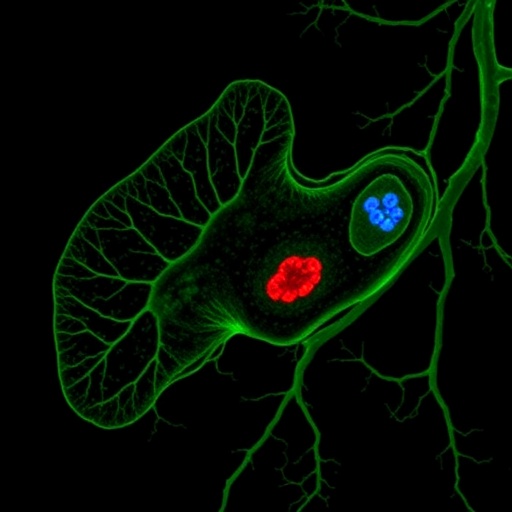
In the evolving landscape of pediatric oncology, hepatoblastoma has emerged as the most prevalent primary liver cancer affecting infants and young children, a phenomenon that has drawn increasing global attention over the past three decades. This surge in hepatoblastoma cases worldwide has intensified efforts to unravel its underlying causes, yet despite significant progress in genomic and epigenomic research, a definitive etiology remains elusive. A new comprehensive study spearheaded by Voskamp, Nelson, and Speck, published in Pediatric Research in November 2025, offers groundbreaking insights into the genetic underpinnings of hepatoblastoma, shedding light on potential diagnostic, prognostic, and therapeutic avenues that could redefine clinical management for this rare malignancy.
Hepatoblastoma, although rare, ranks as a significant clinical challenge due to its aggressive nature and the limited understanding of its molecular drivers. Traditional diagnostic approaches have relied heavily on imaging and histopathological analysis, but these methods often fail to predict disease trajectory or treatment responsiveness accurately. The study focuses on identifying specific genetic mutations and gene expression patterns that could serve as robust biomarkers, facilitating earlier diagnosis and better stratification of patients according to risk profiles, which is crucial for tailoring individualized treatment regimens.
The research covers an extensive analysis of tumor biopsies from a diverse pediatric cohort, integrating whole-genome sequencing, transcriptomics, and epigenetic profiling. This multi-omics approach has unveiled a complex network of genetic alterations, prominently featuring mutations in genes linked to the Wnt/β-catenin signaling pathway, which is well-known for its role in cell proliferation and differentiation. Aberrations in this pathway have been recurrently implicated in hepatoblastoma tumorigenesis, and the current findings reinforce the notion that targeting this pathway could interrupt cancer progression at a molecular level.
Beyond the Wnt/β-catenin axis, the investigators identified novel mutations in chromatin remodeling genes and DNA repair pathways, suggesting that hepatoblastoma development might be fueled by a broader spectrum of genetic instability than previously appreciated. These discoveries hint at a multifaceted oncogenic landscape, where disruptions in genome maintenance mechanisms contribute to tumor heterogeneity and potentially influence response to chemotherapeutic agents.
The team further explored the epigenetic modifications accompanying the genetic alterations, highlighting methylation changes that could act as regulatory switches for oncogene activation and tumor suppressor gene silencing. Such epigenetic signatures may hold promise as non-invasive biomarkers detectable through liquid biopsy techniques, which could revolutionize monitoring disease progression and treatment efficacy without the need for repeated tissue sampling.
Therapeutically, this study paves the way for precision medicine by pinpointing molecular targets that can be exploited for drug development. Inhibitors aimed at the aberrant Wnt signaling components, alongside agents that restore chromatin remodeling functions, are under active investigation. Remarkably, some of these therapeutic candidates have shown efficacy in preclinical models, underscoring the translational potential of the research to improve survival outcomes in affected children.
Moreover, the prognostic implications of the identified gene signatures are significant. By correlating specific genetic alterations with patient outcomes, the researchers have developed a predictive framework that could inform clinical decision-making. High-risk genetic profiles highlight patients who may benefit from intensified therapy or novel treatment combinations, whereas low-risk profiles might avoid overtreatment and associated toxicities, thereby improving the quality of life during and after cancer therapy.
This genetic stratification also provides a valuable tool for future clinical trials, enabling more accurate patient selection and potentially accelerating the evaluation of targeted therapies. The integration of molecular diagnostics into standard care protocols promises to shift the treatment paradigm from a one-size-fits-all approach to one defined by individual tumor biology.
Beyond its immediate clinical implications, this work contributes to the broader understanding of pediatric oncology by emphasizing the importance of genetic and epigenetic interactions in childhood cancers. The findings resonate with parallel research in other pediatric malignancies, where similar pathways appear to govern disease behavior, suggesting opportunities for cross-cutting therapeutic innovations.
The study’s comprehensive approach reflects an appreciation of the complexity inherent in cancer biology, moving beyond single-gene analyses to embrace the dynamic interplay of genetic networks and epigenetic landscapes. Such holistic investigation is essential for uncovering the multifactorial nature of cancer and for devising strategies capable of overcoming the adaptive resilience tumors often exhibit.
Importantly, the identification of potential biomarkers also raises hopes for earlier detection of hepatoblastoma, which is critical given the aggressive course of the disease. Earlier diagnosis could translate into improved curative rates, reducing the reliance on extensive chemotherapy and liver transplantation, both of which carry significant risks and long-term sequelae.
Looking ahead, the prospect of integrating genomic, epigenomic, and proteomic data into comprehensive diagnostic platforms heralds a new era in hepatoblastoma management. By enabling real-time monitoring of tumor evolution and therapeutic resistance, such advanced methodologies may eventually transform hepatoblastoma from a highly challenging cancer into a manageable chronic condition or even curable disease.
The researchers emphasize the necessity of continued collaboration across pediatric oncology centers worldwide to validate these findings in larger, ethnically diverse populations. Such efforts are vital to ensure the generalizability of the genetic markers and to optimize the delivery of personalized medicine across different healthcare settings.
In summary, the study conducted by Voskamp, Nelson, and Speck represents a landmark in hepatoblastoma research, synthesizing cutting-edge genomic techniques with clinical insights to chart a path toward precision oncology in pediatric liver cancer. As the global burden of hepatoblastoma continues to rise, these discoveries offer a beacon of hope for affected children and their families through improved diagnostics, prognostics, and targeted therapeutic interventions.
Subject of Research: Hepatoblastoma genetic signatures, diagnostic and prognostic biomarkers, and therapeutic targets.
Article Title: Hepatoblastoma: an investigation of diagnostic, prognostic, and therapeutic gene targets and biomarkers.
Article References:
Voskamp, S., Nelson, J. & Speck, K.E. Hepatoblastoma: an investigation of diagnostic, prognostic, and therapeutic gene targets and biomarkers. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04492-1
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41390-025-04492-1
Keywords: Hepatoblastoma, pediatric liver cancer, genetic mutations, Wnt/β-catenin signaling, epigenetics, biomarkers, precision medicine, pediatric oncology