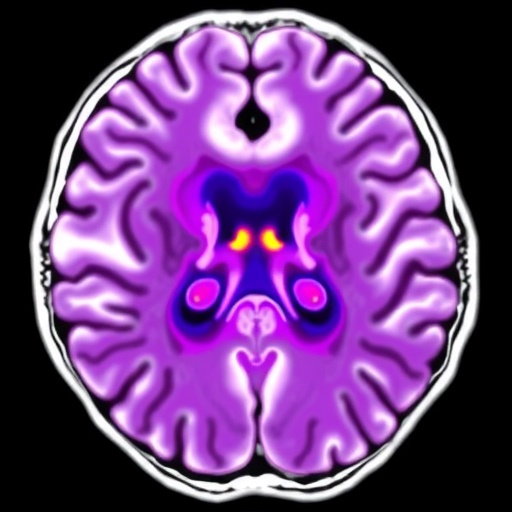
In a groundbreaking study published in the 2025 edition of BMC Psychiatry, researchers have unveiled compelling evidence linking non-alcoholic fatty liver disease (NAFLD) to disruptions in the brain’s glymphatic system, a vital network responsible for waste clearance and overall neurological health. Utilizing an advanced magnetic resonance imaging (MRI) technique, diffusion tensor imaging along the perivascular space (DTI-ALPS), the team explored how pre-cirrhotic NAFLD patients experience significant alterations that may contribute to cognitive decline.
The glymphatic system, a brain-wide pathway that facilitates the convective movement of cerebrospinal fluid through perivascular spaces, plays a crucial role in clearing metabolic waste and maintaining homeostasis. Dysfunction of this system has been increasingly implicated in neurodegenerative diseases and cognitive impairments, but its relationship with systemic metabolic disorders such as NAFLD has remained largely elusive until now.
In this cross-sectional analysis, 43 male patients diagnosed with pre-cirrhotic NAFLD, averaging 38 years of age, were compared with 23 controls matched for age, sex, and education. Both groups underwent rigorous cognitive assessments alongside specialized diffusion tensor imaging to calculate the ALPS index—a quantitative measure reflecting glymphatic function by evaluating water diffusivity along perivascular spaces.
Results from the study highlighted a marked reduction in the ALPS index within the NAFLD cohort relative to their healthy counterparts, even after controlling for confounding factors such as age, sex, and body mass index (BMI). This decline suggests an impaired clearance mechanism within the brain’s glymphatic system, potentially exposing neural tissue to buildup of harmful substances and toxins.
Further analysis revealed increased diffusivity along projection fibers in the direction of the y-axis among NAFLD patients—a finding indicative of microstructural abnormalities possibly linked to neuroinflammation or subtle white matter damage. These changes were robust, underscoring that NAFLD’s impact may extend beyond the liver, influencing neurological integrity at a microstructural level.
Correlations drawn between the ALPS index and cognitive performance reinforced the clinical significance of the findings. Notably, lower ALPS values were associated with poorer scores on the Mini-Mental State Examination (MMSE) and the clock drawing test, two widely recognized metrics for evaluating global cognition and executive function. This association hints at a potential mechanistic link between glymphatic dysfunction and the early cognitive deficits observed in NAFLD patients.
Intriguingly, a positive correlation was observed between the ALPS index and abdominal visceral adipose tissue area, a clinical indicator of fat accumulation around internal organs implicated in metabolic syndrome. This relationship persisted after adjusting for critical variables and suggests a complex interplay between visceral obesity, liver pathology, and cerebral fluid dynamics.
The implications of this study are far-reaching. By demonstrating that glymphatic system function is compromised in NAFLD individuals prior to cirrhosis, the researchers open new avenues for understanding the neurocognitive sequelae of metabolic liver disease. The glymphatic pathway emerges as not only a biomarker but also a potential therapeutic target for mitigating brain dysfunction in these patients.
Moreover, the use of DTI-ALPS offers a non-invasive, sensitive approach to detect early glymphatic alterations, making it a promising tool for longitudinal monitoring. This could enable clinicians to identify individuals at heightened risk for cognitive decline and intervene before irreversible neurological damage occurs.
The study also adds to the growing consensus that systemic metabolic disturbances wreak havoc on brain health. NAFLD, traditionally viewed through the lens of hepatology, now demands a multidisciplinary approach encompassing neurology and psychiatry, emphasizing brain–liver crosstalk in disease pathogenesis.
One pivotal unanswered question is whether glymphatic dysfunction is a cause or consequence of NAFLD-related cognitive impairment. Longitudinal studies are essential to unravel this temporal relationship and to establish causal pathways. Additionally, it remains to be seen if therapeutic strategies aimed at restoring glymphatic flow might reverse or alleviate cognitive deficits in this population.
The researchers caution that despite the robust findings, their preliminary study is limited by its cross-sectional design and the relatively small sample size. Future research with larger cohorts and diverse demographics will be critical to validate and extend these observations.
The potential for this research to go viral lies in its capacity to reshape our understanding of a common metabolic disorder’s impact on brain health. With NAFLD prevalence soaring globally in tandem with obesity rates, uncovering hidden neurological vulnerabilities holds substantial public health importance.
In conclusion, this pioneering work elucidates a novel pathway by which NAFLD may contribute to cognitive dysfunction: through the alteration of glymphatic clearance mechanisms as detected by advanced MRI techniques. It challenges medical communities to broaden their perspective on metabolic diseases and incorporate neuroimaging biomarkers into routine assessments. As ongoing investigations deepen our comprehension, hope rises for tailored interventions to protect brain function amidst growing liver health challenges.
Subject of Research: Alterations in glymphatic system function in patients with non-alcoholic fatty liver disease (NAFLD) and their relationship with cognition and clinical indicators.
Article Title: Glymphatic alteration in NAFLD patient: a preliminary magnetic resonance imaging study based on DTI-ALPS
Article References: Shu, K., Chen, S., Meng, S. et al. Glymphatic alteration in NAFLD patient: a preliminary magnetic resonance imaging study based on DTI-ALPS. BMC Psychiatry 25, 968 (2025). https://doi.org/10.1186/s12888-025-07432-9
Image Credits: AI Generated