In a groundbreaking study poised to reshape therapeutic strategies for early-stage HER2-positive breast cancer, researchers have delved deep into the genomic subtypes that drive differential responses to preoperative chemotherapy combined with HER2-targeted agents. Published in BMC Cancer, this investigation bridges cutting-edge genomic classification with clinical pathology to unearth biomarkers predictive of treatment efficacy, spotlighting the promise of personalized medicine in combating this aggressive cancer subtype.
HER2-positive breast cancer, characterized by overexpression of the human epidermal growth factor receptor 2, has traditionally posed significant challenges due to its aggressive nature and variable response to standard therapies. The integration of neoadjuvant chemotherapy (NAC) with HER2-directed biologics has been established as a pivotal approach. Yet, patient responses vary markedly, underscoring the urgent need to decode underlying molecular and pathological determinants that forecast treatment outcomes.
The research cohort comprised 186 consecutive early-stage HER2-positive breast cancer patients verified by immunohistochemistry (IHC) and fluorescence in situ hybridization (FISH). Among them, 167 patients with available biopsy specimens received NAC combined with HER2-targeted regimens. Utilizing robust molecular assays—specifically MammaPrint and Blueprint platforms—the investigators stratified tumors into intrinsic genomic subtypes. This granular classification permitted a nuanced evaluation of tumor biology beyond conventional hormone receptor status.
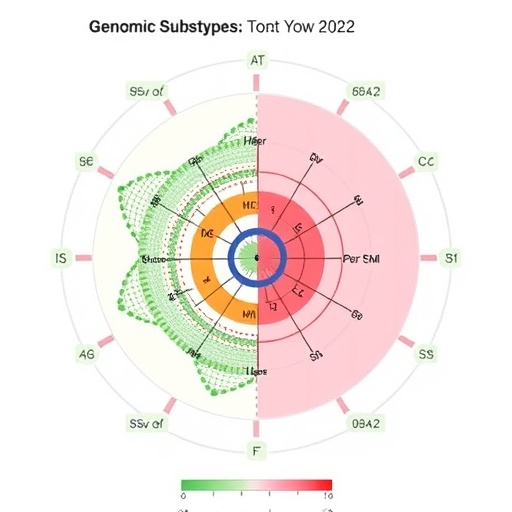
Analysis of 124 patients with identifiable intrinsic subtypes revealed heterogeneous distribution: Luminal-A, Luminal-B, HER2-enriched, and Basal subtypes accounted for distinct portions of the cohort. Intriguingly, pathological complete response (pCR), a critical indicator of favorable prognosis akin to eradication of invasive tumor cells, was significantly elevated in the HER2-enriched subgroup compared to non-HER2 subtypes. Statistical rigor affirmed these differences, with p-values underscoring the robustness of this association.
A salient discovery highlighted that high-intensity HER2 protein expression, as quantified by detailed whole-slide imaging of IHC staining, functioned as an independent predictor of pCR. This aligns with the biological premise that greater HER2 receptor abundance potentiates susceptibility to targeted therapies. Parallelly, the Blueprint-defined HER2 intrinsic subtype emerged as a standalone prognostic factor, augmenting the predictive landscape for therapeutic response.
Interestingly, hormone receptor status stratification revealed that none of the estrogen receptor (ER)-negative patients harbored Luminal subtypes, whereas more than half of the ER-positive patients surprisingly exhibited the HER2-enriched subtype. This finding nuances the conventional binary classification of breast cancers and propels the importance of genomic profiling to tailor treatments comprehensively.
Longitudinal survival analytics provided further insights, with five-year distant disease–free survival (DDFS) rates varying by subtype: Luminal-A patients enjoyed the highest DDFS at over 92%, whereas Basal and HER2 subtypes recorded slightly lower but still substantial survival probabilities. These metrics validate the prognostic relevance of molecular stratification beyond immediate treatment response, shaping long-term clinical management.
Equally noteworthy was the observation of subtype plasticity. In a subset of patients whose tumors were assessed both pre- and post-surgery, nearly half exhibited a shift in intrinsic subtype. This dynamic genomic evolution under therapeutic pressure underscores challenges in static classification and calls for adaptive strategies integrating serial biopsies to refine prognostication and treatment tailoring across the disease timeline.
Methodologically, the study leveraged the concordance of MammaPrint gene expression profiling with Blueprint’s intrinsic subtype determinations, reinforcing the robustness of combining gene signature tools. This synergistic approach, complemented by meticulous histopathological evaluation including HER2 IHC intensity quantification, exemplifies the power of integrated diagnostics.
Clinically, these findings propel the paradigm shift toward biomarker-driven oncology. Identifying patients with high HER2 intensity and HER2 intrinsic subtype tumors primes clinicians to predict which individuals are most likely to achieve pCR, guiding decisions on treatment intensification or de-escalation. Such precision medicine approaches promise to enhance survival outcomes while minimizing unnecessary toxicity.
The translational implications extend to drug development pipelines, where understanding the molecular underpinnings of response and resistance can inform next-generation HER2-targeted therapeutics and combination regimens. Moreover, recognizing the fluidity of tumor genomics highlights the necessity for dynamic treatment algorithms embracing real-time molecular monitoring.
Notably, this study also contributes to the growing discourse on heterogeneity within HER2-positive disease. It challenges the notion of a monolithic entity, instead revealing diverse molecular landscapes that critically influence chemotherapy and targeted therapy synergy. This knowledge fuels the pursuit of customized interventions that transcend current one-size-fits-all protocols.
Future investigations building on these insights are poised to unravel mechanisms driving subtype shifts and intrinsic resistance pathways. Integrating multi-omics analyses, including proteomics and single-cell sequencing, may illuminate tumor microenvironment interactions pivotal to treatment response variability. Such integrative frameworks will be central to evolving breast cancer therapeutics.
In sum, Imamura and colleagues have delivered compelling evidence that genomic subtyping, particularly through MammaPrint and Blueprint platforms, combined with clinicopathological assessment of HER2 intensity, revolutionizes the predictive accuracy for neoadjuvant treatment outcomes in early HER2-positive breast cancer. Their work charts a course toward refined, individualized therapies maximizing efficacy while mitigating overtreatment.
This research heralds a new frontier in the oncological management of HER2-positive breast cancers, integrating molecular precision with practical clinical metrics. As the field advances, these insights will become indispensable instruments in the clinician’s arsenal, translating into tangible patient benefits and advancing the overarching goal of personalized cancer care.
Subject of Research: Genomically determined subtypes and clinicopathological features as predictors of neoadjuvant chemotherapy combined with HER2-targeted therapy efficacy in early-stage HER2-positive breast cancer.
Article Title: Genomically determined subtypes and clinicopathological features as predictors of the efficacy of preoperative chemotherapy combined with HER2-targeted therapy for early-stage HER2-positive breast cancer
Article References: Imamura, S., Mori, K., Yasojima, H. et al. Genomically determined subtypes and clinicopathological features as predictors of the efficacy of preoperative chemotherapy combined with HER2-targeted therapy for early-stage HER2-positive breast cancer. BMC Cancer 25, 1707 (2025). https://doi.org/10.1186/s12885-025-15133-5
Image Credits: Scienmag.com
DOI: 10.1186/s12885-025-15133-5