In a groundbreaking study published in Cell Death Discovery, researchers have unveiled a novel molecular mechanism that heightens the radiosensitivity of head and neck squamous cell carcinoma (HNSCC) by modulating ferroptosis, a unique form of regulated cell death. This innovative research illuminates the role of G9a deficiency in activating TMEM27, catalyzing ferroptosis and offering promising therapeutic avenues for improving treatment outcomes in one of the most aggressive and treatment-resistant cancers.
Head and neck squamous cell carcinoma remains a major clinical challenge due to its aggressive nature and often poor response to conventional therapies such as radiotherapy. Despite advancements in technology and precision oncology, tumor resistance frequently impedes effective radiotherapeutic eradication, highlighting an urgent need for identifying novel molecular targets that sensitize cancer cells to radiation-induced damage.
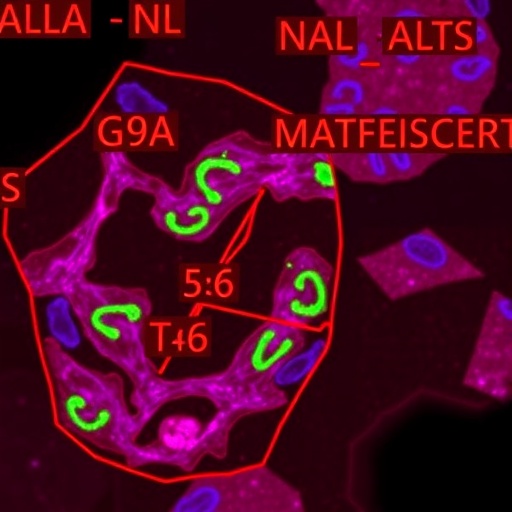
The crux of the study lies in the epigenetic regulation carried out by the histone methyltransferase G9a, an enzyme known for its pivotal role in chromatin remodeling and gene expression silencing via histone H3 lysine 9 dimethylation (H3K9me2). Notably, the researchers discovered that G9a deficiency leads to a marked upregulation of TMEM27, a transmembrane protein previously underexplored in the context of ferroptosis and tumor radiosensitivity.
Ferroptosis, characterized by the iron-dependent accumulation of lipid peroxides to lethal levels, represents a distinct form of cell death differentiated from apoptosis or necrosis. By steering tumor cells toward this catastrophic lipid peroxidation pathway, radiosensitivity can be drastically amplified, rendering cancer cells more vulnerable to the damaging effects of ionizing radiation.
Employing rigorous in vitro and in vivo methodologies, the investigators demonstrated that knocking down G9a increased TMEM27 expression, which, in turn, induced ferroptotic cell death pathways. This activation of ferroptosis primes HNSCC cells for enhanced radiation-induced cytotoxicity, effectively overcoming the typical radioresistance mechanisms that blunt treatment efficacy.
The molecular interplay highlighted by the study delineates how epigenetic deregulation through G9a deficiency alters the ferroptotic landscape of cancer cells. TMEM27 acts as a critical mediator, orchestrating lipid peroxidation processes and iron metabolism to tip the balance toward ferroptosis. This intersection of epigenetics and ferroptosis paves the way for biomarker development and targeted therapy combinations.
Moreover, the research harnessed cutting-edge gene editing technologies and state-of-the-art lipidomic analyses to substantiate the role of TMEM27 as a facilitator of ferroptosis. These methodologies allowed detailed mapping of cellular lipid alterations and iron homeostasis disruptions under variable G9a expression conditions, solidifying a causal relationship between G9a deficiency, TMEM27 activation, and ferroptotic susceptibility.
Importantly, the enhanced radiosensitivity observed was not confined to cell culture. Animal models of HNSCC treated with radiation exhibited significantly improved tumor control when G9a activity was inhibited, confirming translational relevance. This finding is particularly impactful, as it suggests that modulating G9a and TMEM27 could improve radiotherapy outcomes in patients.
The implications of this study extend beyond head and neck cancers. Given that ferroptosis is emerging as a critical vulnerability in diverse tumor types, the regulatory axis of G9a and TMEM27 might represent a universal paradigm for radiosensitization and combination therapies. Targeting epigenetic regulators to modulate ferroptotic pathways opens untapped therapeutic potential across oncology.
Furthermore, this research challenges the conventional understanding of radiotherapy resistance by integrating epigenetic control mechanisms with metabolism-driven cell death processes. It underscores the complexity of tumor biology wherein histone modification states directly dictate cellular susceptibility to oxidative damage, mediated by ferroptotic triggers.
The intersectionality of G9a deficiency and TMEM27 function also creates opportunities for novel drug development. Small-molecule inhibitors or gene therapy approaches could be designed to selectively reduce G9a expression or mimic TMEM27 activation, thereby maximizing ferroptosis induction prior to radiotherapy. Such combinational strategies may potentiate clinical responses while minimizing adverse effects.
The study raises critical questions for future research, including elucidating the precise downstream signaling pathways engaged by TMEM27, its interactions with other ferroptosis regulators, and its role in the tumor microenvironment. Additionally, the reversibility and specificity of G9a-mediated epigenetic changes warrant comprehensive exploration to fully harness this mechanism for personalized medicine.
Clinically, these findings advocate for diagnostic assessments of G9a and TMEM27 expression profiles in patients slated for radiotherapy, potentially allowing clinicians to stratify patients by their likelihood of response. Personalized radiosensitization regimens could thereby enhance therapeutic indices and reduce unnecessary exposure in radioresistant cases.
Furthermore, this investigation contributes to the growing recognition of ferroptosis as a therapeutic frontier. By linking epigenetics—traditionally associated with gene silencing—and ferroptotic cell death, the study bridges distinct biological domains to formulate a coherent strategy for combatting treatment-refractory cancers.
In essence, this research embodies a paradigm shift. Targeting chromatin-modifying enzymes to manipulate non-apoptotic cell death pathways may revolutionize therapeutic approaches, moving beyond the limitations of current radiotherapy protocols and enhancing patient survival in head and neck squamous cell carcinoma.
Ultimately, the elucidation of the G9a-TMEM27-ferroptosis axis reveals new molecular vulnerabilities that can be exploited to surmount radioresistance, a perennial obstacle in oncology. This insight catalyzes translational research efforts aimed at integrating epigenetic and metabolic targeting modalities into the clinical management of malignancies.
As head and neck cancers continue to impose substantial morbidity worldwide, advancements such as this not only offer hope but concretely propose actionable pathways to improve clinical outcomes. The fusion of epigenetic modulation and ferroptotic manipulation epitomizes the next generation of cancer therapy innovation.
Subject of Research: Head and neck squamous cell carcinoma, ferroptosis, radiosensitivity, epigenetic regulation, G9a, TMEM27
Article Title: G9a deficiency activates TMEM27 to promote ferroptosis and enhances radiosensitivity in head and neck squamous cell carcinoma
Article References:
Hu, J., Qiu, Y., Yuan, W. et al. G9a deficiency activates TMEM27 to promote ferroptosis and enhances radiosensitivity in head and neck squamous cell carcinoma. Cell Death Discov. 11, 517 (2025). https://doi.org/10.1038/s41420-025-02805-1
Image Credits: AI Generated
DOI: 10 November 2025