In recent years, the intricate relationship between microbial presence and cancer development has gathered unprecedented scientific attention, with Fusobacterium nucleatum emerging as a pivotal player in oral oncogenesis. This groundbreaking revelation reshapes our understanding of how microorganisms interact with human cellular pathways, potentially driving malignant transformation in oral tissues. The latest research, outlined by Srivastava and Kumar in their article published in Medical Oncology, provides compelling evidence linking Fusobacterium nucleatum to altered cancer pathways within the oral cavity, offering significant insight into microbial oncogenesis mechanisms.
Oral cancer, a formidable global health challenge, has traditionally been associated with risk factors such as tobacco, alcohol, and human papillomavirus. However, this emerging body of research underscores the bacterial influence, particularly that of Fusobacterium nucleatum, a Gram-negative anaerobic bacterium known for inhabiting the oral cavity and implicated in periodontal disease. Its role extends beyond infection, implicating it in the molecular dialogues that dictate tumor behavior. The study presents molecular data illustrating how Fusobacterium nucleatum modulates host cellular environments, promoting carcinogenic pathways through complex mechanisms.
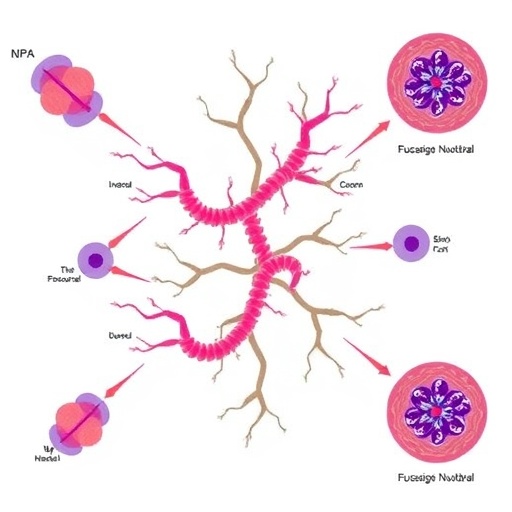
Central to the oncogenic potential of Fusobacterium nucleatum is its ability to adhere to and invade epithelial cells lining the oral mucosa. The bacterium expresses an array of virulence factors, including FadA adhesin, which facilitates its attachment and invasion into host cells. This interaction disrupts cellular signaling and immune responses, enabling a microenvironment conducive to tumorigenesis. The investigation reveals that FadA binding activates β-catenin signaling, a pathway notoriously involved in cell proliferation and cancer development, thereby directly influencing cell cycle dynamics and apoptotic resistance in oral epithelial cells.
Moreover, Fusobacterium nucleatum exerts a profound effect on the immune microenvironment within the oral cavity. It induces an immunosuppressive milieu by modulating immune checkpoints and recruiting regulatory immune cells that dampen the anti-tumoral immune response. The suppression of cytotoxic T cells and natural killer cells facilitates immune evasion by malignant cells, a hallmark of cancer progression. Srivastava and Kumar delineate how this immune modulation is orchestrated via bacterial components like lipopolysaccharides, which engage toll-like receptors signaling pathways, thus triggering chronic inflammation that accelerates carcinogenesis.
The phenomenon of microbial oncogenesis, as exhibited by Fusobacterium nucleatum, also involves metabolic reprogramming of the host cells. The bacterium’s interaction alters cellular metabolism, leading to an acidic tumor microenvironment favorable for cancer cell survival and invasion. The research details how shifts in glycolytic pathways and production of short-chain fatty acids contribute to this metabolic landscape, which not only supports tumor growth but also hinders therapeutic efficacy by creating resistance to chemotherapeutic agents.
Epigenetic modifications represent another dimension of Fusobacterium nucleatum’s impact on oral cancer pathways. The bacterium influences DNA methylation patterns and histone modifications in epithelial cells, leading to silencing of tumor suppressor genes and activation of oncogenes. This epigenetic dysregulation perpetuates malignant transformation and tumor progression. The study highlights the importance of these changes, linking bacterial infection to the disruption of genomic stability and chromatin architecture, which are critical in cancer development.
Advanced molecular techniques employed in this research use high-throughput sequencing and proteomic analyses to delineate the host-microbe interactions at an unprecedented resolution. These approaches reveal the complex network of signaling cascades altered by Fusobacterium nucleatum, including the upregulation of inflammatory cytokines such as IL-6 and TNF-α. This cytokine storm consequently promotes angiogenesis and tumor cell migration, underscoring the direct contribution of bacterial presence to tumor aggressiveness and metastasis potential.
Understanding the role of Fusobacterium nucleatum in oral cancer also opens new avenues for diagnostic and therapeutic strategies. The bacterium could serve as a biomarker for early detection, given its specific association with precancerous lesions and malignancies. Additionally, targeting Fusobacterium nucleatum directly or disrupting its pathogenic mechanisms presents a promising therapeutic strategy. Antimicrobial agents combined with immunomodulatory drugs may enhance treatment responses, according to the pathways elucidated in this study.
The implications of this research transcend oral oncology, highlighting a broader paradigm in cancer biology wherein microbial components are integral to tumor dynamics. Fusobacterium nucleatum’s systemic impact, observed in colorectal and pancreatic cancers, suggests a shared microbial oncogenesis mechanism. This highlights the necessity for cross-disciplinary research integrating microbiology, immunology, and oncology to fully unravel the complexities of cancer pathogenesis influenced by microbial ecosystems.
Critically, the study advocates for more comprehensive clinical trials to validate the efficacy of interventions targeting Fusobacterium nucleatum in clinical oncology. The potential for probiotic, antibiotic, or immunotherapeutic approaches modeled around microbial manipulation could revolutionize the current cancer treatment landscape. Furthermore, personalized medicine approaches considering a patient’s oral microbiome composition could lead to individualized and more effective cancer care regimens.
The research by Srivastava and Kumar represents a seminal advancement in understanding oncogenic microbial influence, emphasizing the need to reassess traditional cancer models with microbial integrative perspectives. It challenges the oncology community to consider infection not merely as a collateral factor but as a driving component of cancer biology. This paradigm shift catalyzes renewed focus on microbial ecology within tumor microenvironments as a source of groundbreaking therapeutic targets.
In conclusion, the elucidation of Fusobacterium nucleatum’s multifaceted influence on oral cancer pathways exemplifies the intricate interplay between microbes and malignancy. From modulating signaling pathways to remodeling immune landscapes and reshaping host metabolism and epigenetics, this bacterium exemplifies a sophisticated oncogenic entity embedded within the tumor microenvironment. This comprehensive understanding promises to fuel novel diagnostics, preventive measures, and therapies that could significantly alter outcomes for oral cancer patients worldwide.
These findings should resonate beyond the scientific community, highlighting the importance of oral hygiene and microbial management as potential preventative measures against oral carcinogenesis. The recognition of Fusobacterium nucleatum as a bona fide oncogenic microorganism calls for public health initiatives aimed at mitigating bacterial-induced cancer risks, potentially reducing the global burden of oral malignancies.
As the scientific world delves deeper into microbial-associated cancers, Fusobacterium nucleatum stands at the forefront of this emerging field, symbolizing both the complexity and opportunity inherent in microbial oncogenesis research. The work of Srivastava and Kumar thus marks a critical milestone, paving the way for innovative, microbe-centered cancer therapeutics and prevention strategies that promise to reconfigure future oncology paradigms.
Subject of Research: Impact of Fusobacterium nucleatum on oral cancer pathways and microbial oncogenesis.
Article Title: Microbial oncogenesis: the impact of Fusobacterium nucleatum on oral cancer pathways.
Article References:
Srivastava, S., Kumar, S. Microbial oncogenesis: the impact of Fusobacterium nucleatum on oral cancer pathways. Med Oncol 43, 18 (2026). https://doi.org/10.1007/s12032-025-03150-0
Image Credits: AI Generated