In the ever-evolving landscape of psychiatric research, major depressive disorder (MDD) has long troubled clinicians and neuroscientists alike with its complex symptomatology and pervasive impact across populations. While it is widely recognized as one of the leading causes of disability worldwide, the undercurrents driving its expression and treatment outcomes remain enigmatic. A groundbreaking study published in early 2025 has illuminated a transformative perspective by establishing sex not merely as a demographic detail but as an essential biological variable profoundly influencing the neurofunctional substrates of depression. This study employs cutting-edge functional neuroimaging to unravel how depression manifests differently in males and females, potentially revolutionizing diagnostic and therapeutic frameworks.
The impetus behind this investigation stems from a well-documented yet insufficiently dissected observation: depression does not affect everyone equally. Epidemiological data have long noted that women are nearly twice as likely as men to develop MDD, presenting with distinctive symptom clusters and disparate responses to conventional antidepressants. Despite these clinical observations, sex differences have often been relegated to peripheral status rather than integrated into the core of pathophysiological paradigms. Sridhar, Struckmann, Johnson, and colleagues challenge this reductive approach by deploying functional magnetic resonance imaging (fMRI) to assay brain activity patterns underpinning depression across sexes. Their findings underscore the necessity of incorporating sex as a pivotal variable when interpreting neurobiological data and tailoring interventions.
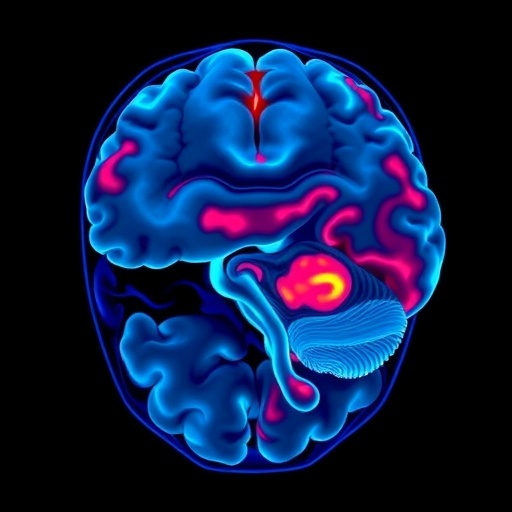
Functionally, MDD involves dysregulation within neural circuits governing mood regulation, reward processing, cognitive control, and emotional salience. However, until this study, the degree to which these circuit disruptions vary by sex remained murky at best. Utilizing advanced imaging protocols with rigorous statistical modeling, the researchers uncovered that women with depression demonstrate heightened activity in limbic regions such as the amygdala and hippocampus—areas integral to emotional memory and processing—whereas men exhibit more pronounced atypical activation in prefrontal cortex nodes responsible for executive functioning and behavioral regulation. These distinctions offer a neural explanation for clinical observations: women with MDD often report affective symptoms like sadness and anxiety, whereas men tend toward impairments in concentration and psychomotor slowing.
Beyond functional differences, the team explored connectivity patterns, revealing sex-specific alterations in the coupling between cortical and subcortical regions. In female subjects, disrupted communication between the prefrontal cortex and the striatum—a key component in reward circuitry—correlated with anhedonia severity. Contrastingly, males demonstrated weakened connectivity between prefrontal areas and the amygdala, potentially underlying difficulties with emotional regulation. These nuanced insights into network-level dynamics embody a crucial advance, suggesting that depression is not a monolithic brain disorder but a constellation of sex-influenced neurobiological phenotypes.
Perhaps most compelling, the study addresses a long-standing challenge in psychiatric research: the paucity of reliable biomarkers capable of informing personalized treatment strategies. By differentiating neuroimaging signatures by sex, this research paves the way for precision psychiatry, whereby interventions can be more selectively matched to individual neurofunctional profiles. For instance, women’s heightened limbic reactivity may render them more responsive to pharmacotherapies targeting glutamatergic or serotonergic pathways implicated in emotional processing, whereas men might benefit from neuromodulatory approaches aiming to enhance executive control circuits.
Importantly, these findings also prompt a reevaluation of existing clinical trial designs in depression research. Historically, trials have often underrepresented women or failed to analyze sex-specific outcomes systematically, thereby obscuring potential differences in efficacy and side effect profiles. The revealed sex-dependent neural mechanisms advocate for stratifying study cohorts by biological sex and potentially hormonal status, particularly considering fluctuations across menstrual cycles and their impact on brain function. Failure to do so risks invalidating results and perpetuating a one-size-fits-all therapeutic model that may inadequately serve diverse patient populations.
From a methodological standpoint, the study showcases how sophisticated fMRI analytic techniques, such as resting-state functional connectivity and task-evoked activation paradigms, can dissect complex psychiatric phenotypes. The team leveraged machine learning classifiers to differentiate male and female depression cohorts based on neural data, achieving high predictive accuracy that outperforms traditional clinical assessment scales. This synergy between neuroimaging and computational neuroscience exemplifies the emerging frontier where big data and biological insights converge to deepen our understanding of mental illnesses.
Delving into developmental trajectories, the research further speculates on the interplay of sex hormones and brain maturation processes in shaping vulnerability windows for MDD onset. For example, estrogen’s modulatory effects on synaptic plasticity and neurotransmitter systems might sensitize limbic circuits in females during adolescence, aligning with epidemiological peaks in depression prevalence. Conversely, androgens’ influence on prefrontal cortex development could differentially sculpt male neural substrates, impacting cognitive symptomatology. While causality cannot be fully established, these hypotheses open avenues for integrating endocrinological data into neuropsychiatric models.
The clinical implications extend beyond pharmacology to encompass psychotherapeutic strategies well-suited to sex-specific neural profiles. Women exhibiting hyperactive emotional circuits may derive greater benefits from emotion-focused therapies, such as mindfulness-based cognitive therapy or dialectical behavior therapy, which target affect regulation. In contrast, men’s executive dysfunctions might be ameliorated by interventions emphasizing cognitive remediation and behavioral activation techniques to strengthen task-oriented neural networks. Thus, personalized mental health care could be reimagined through the prism of sex-informed neurobiology.
In parallel, the study advocates for incorporating genetic and epigenetic data that interact with sex to modulate brain function and depression risk. Gene expression differences influenced by sex chromosomes or sex hormone receptors could underlie some of the observed neuroimaging disparities. Epigenetic modifications modulated by environmental stressors might also exhibit sex-dependent patterns, influencing susceptibility and resilience mechanisms. An integrated multi-omic approach thus emerges as a necessary future direction to capture the full complexity of depression pathogenesis.
Moreover, this rigorous analysis highlights the limitations of current diagnostic frameworks grounded in symptom checklists, which often mask underlying biological heterogeneity. By spotlighting sex as a critical dimension, the work urges psychiatric nosology to evolve towards a model informed by neurobiological signatures, potentially leading to the identification of subtypes of depression with distinct etiologies and optimal treatment responses. Such progress would mark a paradigm shift away from symptom-based diagnosis toward a mechanism-based classification.
Ethical considerations also surface in implementing sex-specific interventions. Ensuring equitable access and avoiding reinforcing gender biases will be paramount as personalized psychiatry advances. Additionally, awareness of the intersectionality of sex with other factors such as age, ethnicity and socioeconomic status is critical to developing inclusive research and clinical practices that serve diverse individuals affected by depression.
Overall, this seminal research firmly positions sex as a foundational variable in the neuroscientific investigation of depression. By leveraging sophisticated functional neuroimaging methodologies to dissect sex-specific neural circuitry alterations, it opens pathways toward biologically grounded, precision-guided interventions. The potential to enhance treatment efficacy and reduce the global burden of depressive disorders by acknowledging and addressing sex differences heralds an exciting frontier in psychiatric science.
Future studies building upon these insights are anticipated to integrate longitudinal designs, hormonal assays, and multimodal imaging to capture the dynamic interplay of sex and brain function over time. Such comprehensive approaches promise to unearth causal links and refine our understanding of how sex shapes the trajectory, manifestation and remediation of depression. As the scientific community embraces this paradigm, the vexing mystery of why depression manifests so divergently among men and women may finally begin to unravel, delivering hope for millions worldwide.
Subject of Research: Major depressive disorder and sex differences in functional neuroimaging.
Article Title: Functional neuroimaging highlights sex as a critical variable in depression research.
Article References:
Sridhar, M., Struckmann, W., Johnson, N.D. et al. Functional neuroimaging highlights sex as a critical variable in depression research. Nat. Mental Health (2025). https://doi.org/10.1038/s44220-025-00477-5
Image Credits: AI Generated