In the rapidly evolving landscape of neonatal care, functional echocardiography at the point of care is emerging as a revolutionary tool to assess and manage hemodynamic dysfunction in newborns, particularly those suffering from shock. Neonatal shock remains one of the most critical emergencies that neonatologists confront, often leading to significant morbidity and mortality if not promptly diagnosed and treated. Recent advancements, as highlighted in a comprehensive systematic review and meta-analysis published in Pediatric Research, underscore the transformative potential of functional echocardiography to redefine the management protocols for neonatal shock.
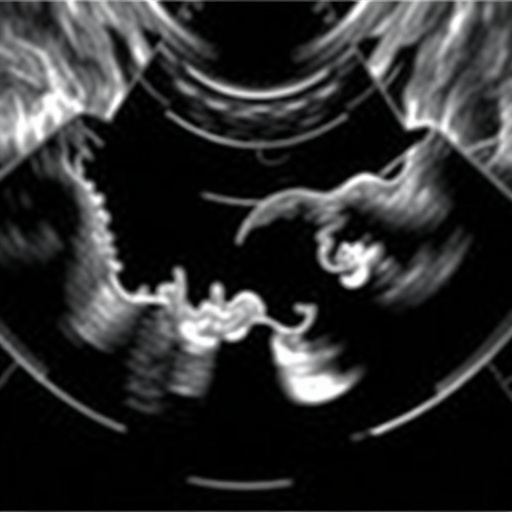
Traditional diagnostic approaches to neonatal hemodynamic instability primarily rely on clinical assessment and indirect markers like blood pressure and urine output, which may not accurately reflect the cardiovascular status in newborns. In contrast, functional echocardiography provides direct visualization of cardiac function, enabling clinicians to evaluate heart contractility, preload, afterload, and cardiac output with unprecedented immediacy and accuracy. This real-time insight is pivotal, especially in the fragile neonatal population, where physiological parameters can fluctuate rapidly, and therapeutic windows are narrow.
The systematic review by Goyal et al. meticulously consolidated data from numerous studies focusing on the utility of functional echocardiography in cases of neonatal shock. Their analysis reveals that integrating this diagnostic modality into routine neonatal intensive care unit (NICU) protocols significantly improves early recognition of shock states and guides targeted interventions. For instance, through the assessment of left ventricular output or superior vena cava flow, clinicians can distinguish between different shock etiologies such as hypovolemic, cardiogenic, or distributive shock. This differentiation is crucial for tailoring treatment strategies, including fluid management, inotrope administration, or vasopressor use.
One of the chief advantages of point-of-care functional echocardiography is its ability to facilitate dynamic monitoring. Neonates with shock require continuous evaluation as their condition evolves, and static measurements often fall short of capturing the complex hemodynamic shifts. Functional echocardiography not only assists in initial diagnosis but also serves as a vital tool to monitor response to therapy. Adjustments in medical management can be done swiftly, guided by imaging findings, thereby reducing the risk of complications associated with over- or under-treatment.
Technological advancements have made echocardiographic equipment more compact, user-friendly, and adaptable to bedside use, perfect for the constrained environment of the NICU. This portability ensures that neonates, who are often too unstable for transport, can undergo hemodynamic assessment without delay. Furthermore, the incorporation of standardized imaging protocols and training programs for neonatologists has enhanced the reproducibility and reliability of functional echocardiographic measurements across different centers, promoting broader adoption and consistent clinical outcomes.
While functional echocardiography opens unprecedented avenues in neonatal cardiology, challenges remain in its implementation. Expertise in image acquisition and interpretation is critical, necessitating dedicated training and credentialing programs for neonatologists. Additionally, integration into existing clinical workflows requires multidisciplinary collaboration, encompassing cardiologists, intensivists, and nursing staff to optimize patient management.
Despite these hurdles, the meta-analytic evidence points to a clear correlation between the use of functional echocardiography and improved survival rates in neonatal shock. The capacity to identify subtle cardiovascular compromise before clinical deterioration allows for preemptive interventions, effectively bridging the gap between detection and treatment. This breakthrough could redefine standards of care and protocols in neonatal critical care units worldwide.
Another important dimension emerging from the study is the role of functional echocardiography in differentiating shock subtypes, which has traditionally been challenging due to overlapping clinical signs in neonates. For example, distinguishing septic shock, which often requires vasopressors and antibiotics, from cardiogenic shock, necessitating inotropic support and fluid restriction, can be fraught with uncertainty. Echocardiographic parameters, including myocardial contractility and chamber dimensions, provide objective criteria to inform clinical decision-making.
The applications extend beyond the management of shock itself; functional echocardiography also contributes to evaluating the impact of various therapeutic modalities. It helps assess the effectiveness of interventions such as volume resuscitation or medication titration, allowing neonatologists to adapt therapies based on physiological responses rather than empiric protocols. This precision medicine approach aligns with broader trends in neonatal care, emphasizing individualized treatment plans.
Importantly, the meta-analysis highlighted in the recent Pediatric Research article sheds light on the safety profile of functional echocardiography in fragile neonates. As a non-invasive technique devoid of radiation exposure, it stands out as a preferable alternative to more invasive hemodynamic monitoring tools like catheterization or central venous pressure measurement, which carry inherent risks.
Educational initiatives and simulation-based training designed to enhance neonatologists’ proficiency in functional echocardiography are gaining momentum, which is crucial for sustaining the momentum of this diagnostic innovation. As the clinical utility becomes better recognized, more institutions are likely to integrate point-of-care echocardiography into their standard protocols, transforming clinical practice.
Looking toward the future, ongoing research aims to refine echocardiographic parameters that predict outcomes and stratify risk among neonates in shock. Biomarker integration with imaging data could further enhance diagnostic accuracy and therapeutic precision. Additionally, automated image processing and the incorporation of artificial intelligence hold promise to democratize expertise and reduce operator dependence.
In conclusion, functional echocardiography represents a breakthrough in neonatal critical care, offering a window into the heart’s function that is both immediate and informative. For neonatologists confronting the unpredictable clinical scenarios of neonatal shock, this technology offers a lifeline, enabling timely, targeted, and dynamic management that can significantly improve infant survival and long-term outcomes.
The systematic review and meta-analysis conducted by Goyal and colleagues not only illuminate the current efficacy of functional echocardiography in neonatal shock but also chart a path for its expanded role in the future of neonatal hemodynamics. As this modality becomes more accessible, it promises to reshape how clinicians diagnose, monitor, and treat the most vulnerable patients at the very beginning of life.
The convergence of technological innovation, clinical expertise, and emerging evidence positions functional echocardiography as an indispensable tool in neonatal medicine. Its adoption marks a paradigm shift from reactive to proactive and precision-driven care, potentially saving countless neonatal lives worldwide.
Subject of Research: Functional echocardiography in the assessment and management of neonatal shock.
Article Title: Role of functional echocardiography in neonatal shock: a systematic review and meta-analysis.
Article References:
Goyal, N., Ananthan, A., Subhadarsini, S. et al. Role of functional echocardiography in neonatal shock: a systematic review and meta-analysis. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04298-1
Image Credits: AI Generated