In a landmark development that could redefine the standard of care in breast cancer treatment, the largest randomized controlled trial to date comparing photon and proton radiation therapies has unveiled compelling findings regarding patient quality of life outcomes. Known as the Radiotherapy Comparative Effectiveness (RadComp) trial, this extensive study enrolled over 1,200 patients across 32 centers in the United States, specifically targeting individuals with non-metastatic, locally advanced breast cancer to evaluate health-related quality of life (HRQoL) after undergoing either of the two radiation modalities.
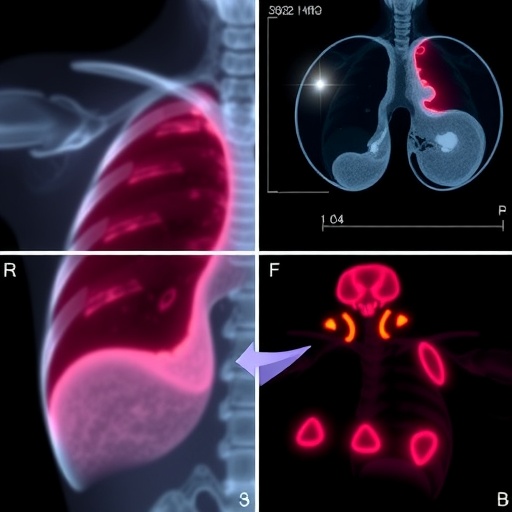
Photon therapy, the longstanding mainstay of external-beam radiation, utilizes high-energy X-rays to eradicate residual cancer cells following surgical interventions. Despite its proven efficacy, the inherent physical characteristics of photons entail the passage of radiation beyond the tumor site, leading to an unavoidable dose distribution that affects surrounding healthy tissues—including crucial organs such as the heart and lungs. This dispersion, albeit minimal, raises concerns about late-onset cardiopulmonary complications, particularly in breast cancer patients who often undergo radiation near sensitive thoracic structures.
In stark contrast, proton therapy leverages charged particles that deposit the majority of their ionizing energy at a precise depth, defined by the Bragg peak phenomenon. This allows oncologists to confine the radiation dose to the tumor and adjacent lymph nodes while sharply limiting exposure to neighboring organs. The physical specificity of protons suggests potential advantages in mitigating long-term adverse events, though the requirement for sophisticated equipment and considerable financial investment has limited its broad implementation in clinical practice.
Against this backdrop, RadComp sought to rigorously assess whether the theoretical dosimetric benefits of proton therapy translate into tangible improvements in patient-centered outcomes. Led by Dr. Shannon MacDonald, a distinguished radiation oncologist and clinical chair of the trial, the study adopted a phase III randomized controlled design to provide high-level evidence. Patients with non-metastatic breast cancer undergoing comprehensive nodal radiation, including those with left-sided and bilateral tumors, were randomized to either proton or photon therapy, ensuring the inclusion of cases at heightened risk for cardiac exposure.
Patient-reported outcomes were meticulously collected using validated instruments designed to capture a multidimensional view of health-related quality of life. Assessments were completed prior to radiation, at treatment completion, and then at one and six months post-therapy. The evaluated domains spanned physical symptoms, emotional and social functioning, as well as overall satisfaction and cosmetic results, thus providing a comprehensive appraisal of treatment impact from the patients’ perspective.
The initial results demonstrate a remarkable equivalence between proton and photon therapies in terms of quality-of-life measures. Patients in both cohorts reported high levels of well-being and satisfaction with their treatments, including comparable perceptions of cosmetic outcomes—a critical consideration given the psychosocial impact of breast cancer therapy. These findings underscore the robustness of contemporary photon therapy protocols and their ability to maintain patient quality of life despite the risks inherent in radiation exposure.
Intriguingly, patients treated with proton therapy exhibited a stronger proclivity to recommend their therapy or choose it again if faced with the decision, a difference observed with strong statistical significance. Dr. MacDonald cautions that such preferences may be influenced by patient perceptions regarding the novelty and advanced nature of proton therapy, rather than reflecting intrinsic clinical advantages. This phenomenon highlights the complex interplay between patient expectations, treatment modality branding, and subjective experience.
A notable observation emerged in the reported incidence of shortness of breath—a symptom potentially indicative of radiation-induced lung toxicity. Patients receiving proton therapy were statistically more likely to report no such symptoms at six months post-treatment. However, this difference did not retain statistical significance after adjusting for multiple comparisons, indicating that while suggestive, the finding requires cautious interpretation and further investigation. Subgroup analyses examining severity grades of respiratory symptoms revealed no meaningful difference between groups, suggesting that overt pulmonary complications are infrequent with either modality.
These data contribute to a growing literature emphasizing the indispensability of patient-reported outcomes in oncological trials. Beyond traditional clinical endpoints such as tumor control and survival, HRQoL metrics provide critical insights into the lived experience of cancer survivors, informing the holistic evaluation of treatment efficacy. Dr. MacDonald advocates for the integration of these measures into future studies to guide nuanced clinical decision-making and health policy.
Beyond the immediate quality-of-life data, RadComp continues to follow participants longitudinally to assess long-term oncologic efficacy and potential cardiac sequelae, endpoints of paramount importance given prior evidence linking radiation exposure to cardiovascular morbidity. The trial’s eventual findings, anticipated in the coming years, are poised to resolve lingering uncertainties regarding the optimal radiation modality that balances maximal tumor control with minimal collateral damage.
The implications of this study are profound for clinical practice and the economics of cancer care. While proton therapy holds promise for dose sparing of critical structures, its high operational costs and limited availability necessitate rigorous justification for routine use. RadComp’s demonstration of comparable quality-of-life outcomes provides evidence supporting the continued use of photon therapy as an effective, accessible option for the majority of breast cancer patients.
As the oncology community awaits headline results on long-term survival and cardiac safety, the current data set offers considerable reassurance that patients can receive top-tier curative radiation through either photon or proton therapy without compromising their quality of life. This knowledge empowers patients and clinicians to engage in informed shared decision-making, balancing the nuances of technology, cost, and patient preference in individualized cancer treatment.
In conclusion, the RadComp trial marks a pivotal advance in comparative oncological research. By harnessing rigorous methodology and incorporating patient voices at its core, it advances our understanding of how state-of-the-art radiation therapies impact the comprehensive wellbeing of breast cancer patients. This work epitomizes the evolution of cancer care from purely clinical efficacy to encompassing patient-centered outcomes, heralding a future where precision in treatment delivery is harmonized with quality of life considerations.
Subject of Research: Comparative effectiveness of photon versus proton radiation therapy in breast cancer treatment focusing on patient-reported quality of life outcomes.
Article Title: Largest Randomized Trial Reveals Equivalent Quality of Life in Photon and Proton Radiation Therapy for Breast Cancer
News Publication Date: September 29, 2025
Web References:
– RadComp trial abstract and session details: https://amportal.astro.org/sessions/pl-01-21644
– American Society for Radiation Oncology (ASTRO) Annual Meeting: http://www.astro.org/annualmeeting
– Study registration: http://bit.ly/ASTRO25-2
Keywords: Breast cancer, Proton therapy, Photon therapy, Radiation therapy, Radiation oncology, Patient-reported outcomes, Quality of life, Clinical trial, Cardiac toxicity, Pulmonary side effects, RadComp trial, Cancer treatment efficacy