In a groundbreaking exploration of pediatric urology, a recent study delves into the imaging techniques employed for diagnosing renal pseudotumors in children. Renal pseudotumors represent a fascinating but often perplexing area in pediatric diagnostics, frequently mimicking true tumors yet having entirely different implications and management protocols. The distinction between these entities is vital, as premature surgical intervention can lead to unnecessary physical trauma in young patients. Consequently, the comprehensive review conducted by Dalkıran et al. sheds much-needed light on this critical aspect of pediatric radiology.
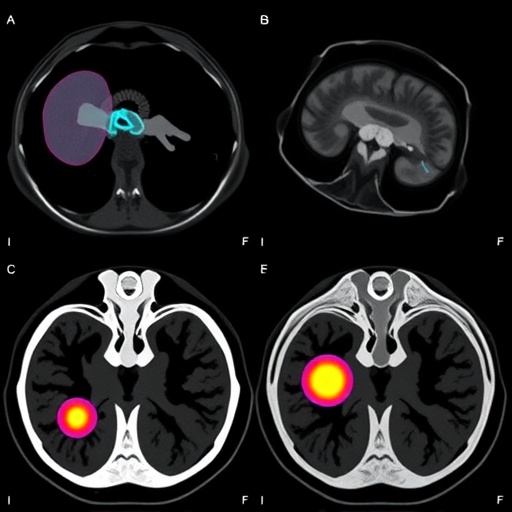
The review begins with an overview of the radiological techniques currently available for differentiating renal pseudotumors from actual renal tumors. Ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI) are amongst the most widely utilized modalities. Each method presents its own strengths and weaknesses, making the understanding of their effective application essential. For example, ultrasonography is advantageous due to its accessibility and lack of ionizing radiation, making it particularly appropriate for children. However, its limitations include operator dependency and difficulty visualizing deep-seated lesions.
On the other hand, CT imaging provides superior detail and clarity in evaluating renal masses but exposes patients to ionizing radiation, raising concerns about long-term effects, especially in the pediatric population. MRI represents a middle ground with its high-resolution images and absence of radiation exposure, allowing for safer assessments. Understanding when and how to deploy these imaging techniques appropriately is essential for accurate diagnosis and timely intervention.
A significant portion of the study is dedicated to the characteristic imaging findings associated with common types of renal pseudotumors. These findings often include notable features such as solid or complex cystic masses, presence of vascularity, and attenuation patterns that can help radiologists determine the nature of the lesion. The review elaborates on various conditions like renal hemorrhage, which may produce a pseudotumor appearance due to hematoma formation, and renal duplications, such as ectopic kidneys or fusion anomalies, that can resemble neoplastic growths.
The authors emphasize the importance of correlating imaging findings with the clinical context. Most notably, clinical history along with laboratory evaluations can provide invaluable clues that help differentiate between benign and malignant processes. For instance, conditions like hyperplasia or xanthogranulomatous pyelonephritis present in ways that may be misconstrued without a comprehensive clinical picture. This integration of clinical and imaging data reinforces a holistic approach to pediatric renal diagnostics.
Another intriguing aspect of the review is its discussion surrounding the evolving role of advanced imaging techniques like elastography and contrast-enhanced ultrasound. These emerging technologies have shown promise in enhancing the diagnostic accuracy of renal lesions, potentially allowing for more nuanced assessments of their biological characteristics without subjecting young patients to invasive procedures. Such advancements not only hold the potential to improve diagnostic pathways but also to facilitate the ongoing research into the biology of renal lesions.
The implications of accurately diagnosing renal pseudotumors cannot be overstated. Incorrect diagnoses can lead to unnecessary surgeries, increased healthcare costs, and significant emotional distress for families. With the advent of precise imaging techniques and a more profound understanding of the differential diagnosis, there is hope for reducing the rate of overtreatment in this vulnerable population.
This review also underscores the importance of interdisciplinary collaboration amongst pediatricians, radiologists, and urologists. By fostering a team-oriented approach to patient care, clinicians can synthesize their expertise, ensuring that every child receives the most informed management plan based on a thorough understanding of their unique clinical picture. Such collaboration not only offers a broader perspective in diagnostic challenges but also enhances the quality of care that pediatric patients receive.
Moreover, the study emphasizes the need for continuous education and training for healthcare professionals involved in pediatric care. Advances in imaging continuously evolve; thus, keeping abreast of these changes can significantly influence patient outcomes. Regular workshops, targeted training, and continued medical education can empower radiologists and clinicians to remain vigilant in distinguishing between renal pseudotumors and true neoplastic processes.
Lastly, the review highlights the potential for more extensive epidemiological studies to understand the prevalence and outcomes associated with renal pseudotumors in children. Establishing a database or registry dedicated to tracking pediatric renal lesions would allow researchers and clinicians to gather critical insight into these often-misunderstood entities. Through such efforts, there is hope for forming a more cohesive understanding of renal pseudotumors and enhancing the overall efficacy of pediatric care.
As the authors conclude, their comprehensive review serves as a clarion call to the medical community about the urgency of refining diagnostic approaches in pediatric renal imaging. With the right tools, knowledge, and collaboration, healthcare professionals can navigate the complexities surrounding renal pseudotumors, ultimately improving the trajectory of care and outcomes for affected children.
Subject of Research: Imaging techniques for renal pseudotumors in children
Article Title: Imaging of renal pseudotumors in children: a comprehensive review.
Article References:
Dalkıran, B., Ozcan, H., Oguz, B. et al. Imaging of renal pseudotumors in children: a comprehensive review.
Pediatr Radiol (2025). https://doi.org/10.1007/s00247-025-06320-4
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s00247-025-06320-4
Keywords: Pediatric radiology, renal pseudotumors, imaging techniques, ultrasonography, computed tomography, magnetic resonance imaging, elastography, interdisciplinary collaboration.