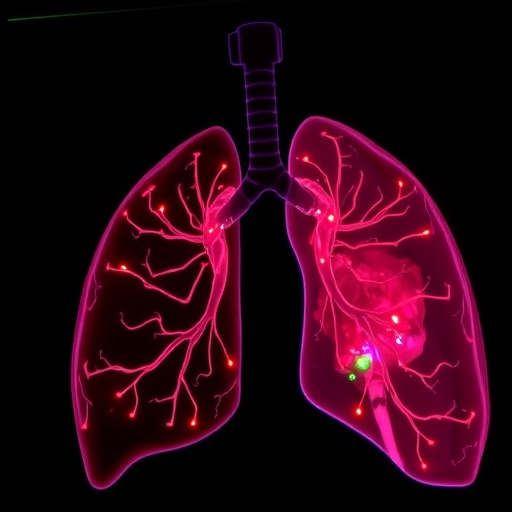
In a groundbreaking study that promises to enhance our understanding of sepsis-induced acute lung injury, researchers Ding, Zhang, and Cai have meticulously unraveled the intricate regulatory mechanisms underlying the roles of hsa-miR-1247-5p and TRIB2. This significant mechanistic inquiry, published in the esteemed journal Scientific Natural, sheds light on the cellular and molecular interactions that exacerbate lung injury during sepsis, a critical condition affecting millions globally.
Sepsis, often the result of an overwhelming immune response to infection, leads to multi-organ dysfunction, with the lungs frequently being one of the first systems to suffer. This research stands out as it dives deep into the uncharted territory of microRNAs and their impact on cellular pathways relevant to acute lung injury. Specifically, the study focuses on hsa-miR-1247-5p, a microRNA that has garnered attention for its potential relevance in various pathological conditions, alongside TRIB2, a known regulator of stress responses and apoptosis in the cells.
The authors conducted a series of experiments using relevant cellular models to investigate how hsa-miR-1247-5p modulates the expression of TRIB2. Through meticulous experimental design, including the use of knockdown and overexpression strategies, the researchers were able to demonstrate that hsa-miR-1247-5p exerts a critical inhibitory effect on TRIB2 expression. This regulation is particularly noteworthy given TRIB2’s established role in promoting cell viability under stress conditions, suggesting that microRNA-mediated suppression might render cells more susceptible to damage during septic challenges.
In their exploration, the research team kept an eye on the signaling pathways activated during sepsis. They illuminated how hsa-miR-1247-5p influences key inflammatory and apoptotic pathways. The interplay between the innate immune response and these signaling cascades is complex, and the researchers emphasize the necessity of understanding how microRNAs can tip the balance towards inflammation or resolution. They provided robust evidence that hsa-miR-1247-5p not only upregulates inflammatory cytokines but also triggers apoptotic markers, advancing the narrative that dysregulation of microRNAs can intensify lung pathology during sepsis.
Further, the study delved into the therapeutic implications of targeting hsa-miR-1247-5p and TRIB2. The researchers propose potential strategies for modulation of hsa-miR-1247-5p levels therapeutically, aiming to provide a novel approach to mitigate acute lung injury in septic patients. With the advent of microRNA-targeting therapies, the possibility of fine-tuning the immune response and preventing lung damage becomes increasingly plausible.
Considering the clinical relevance, the conclusions drawn from this study could stimulate a wave of further research towards the therapeutic implications of hsa-miR-1247-5p modulation in sepsis. The team suggests that future therapies might include the use of synthetic oligonucleotides to inhibit hsa-miR-1247-5p, potentially enhancing TRIB2 activity and thus providing a protective effect against sepsis-induced lung injury.
As the researchers continue to pave the path for subsequent inquiries, the urgency of addressing acute lung injury in the context of sepsis cannot be overstated. The implications of their findings extend beyond academic interest; they provide a hopeful glimpse into new treatment modalities that could save lives. The interconnectivity of hsa-miR-1247-5p, TRIB2, and the inflammatory response underscores the critical nature of investing into microRNA research.
Moreover, this study fits into a growing body of literature that is increasingly acknowledging the implications of non-coding RNAs in disease processes. As we move towards a more integrative understanding of sepsis pathophysiology, the importance of miRNA regulation in cellular homeostasis becomes crystal clear. Researchers in the field will undoubtedly be inspired to investigate other microRNAs that may play comparable roles in sepsis and acute lung injury.
In a larger context, as healthcare practitioners continue to grapple with the repercussions of sepsis—a condition responsible for considerable morbidity and mortality—this research propels the importance of individualized treatments forward. The prospect of personalized medicine tailored towards modulating microRNA levels may not be just a futuristic vision but an impending reality, informed by studies like Ding et al.’s.
The findings encapsulated in this study evoke a familiar yet crucial question: How can we translate molecular insights into clinical practice effectively? This is where the real challenge lies, as validating these findings through clinical trials will ultimately determine their applicability and efficacy in real-world treatments.
In summary, Ding, Zhang, and Cai’s exploration into the roles of hsa-miR-1247-5p and TRIB2 in sepsis-induced acute lung injury not only uncovers novel mechanistic insights but also opens doors to innovative therapeutic strategies. As the scientific community continues to unravel the complexities of sepsis and its dreadful consequences, this investigation stands as a pivotal reference point in the ongoing quest to improve patient outcomes and advance the frontiers of medical science.
Subject of Research: The regulatory role of hsa-miR-1247-5p and TRIB2 in sepsis-induced acute lung injury.
Article Title: Mechanistic study on the regulatory role of hsa-miR-1247-5p and TRIB2 in sepsis-induced acute lung injury.
Article References:
Ding, X., Zhang, B., Cai, S. et al. Mechanistic study on the regulatory role of hsa-miR-1247-5p and TRIB2 in sepsis-induced acute lung injury.
Sci Nat 112, 87 (2025). https://doi.org/10.1007/s00114-025-02033-8
Image Credits: AI Generated
DOI: 10.1007/s00114-025-02033-8
Keywords: hsa-miR-1247-5p, TRIB2, sepsis, acute lung injury, microRNA, inflammatory response, apoptosis, therapeutic strategies.