In recent years, the COVID-19 pandemic has transformed the landscape of public health, leading to a significant emphasis on understanding and diagnosing a complex array of symptoms associated with long COVID, often called Post-Acute Sequelae of SARS-CoV-2 infection (PASC). This shift in focus is critical as millions globally grapple with lingering symptoms long after the acute phase of their infection has passed. A recent study undertaken by a team of researchers, including Azola, Dastgheyb, and Easter, sheds new light on the validity of the PASC score, critically assessing its clinical versus statistical accuracy in diagnosing long COVID.
The PASC score was developed to provide a standardized tool for clinicians to evaluate and efficiently diagnose symptoms of long COVID. It takes into account a variety of factors, including neurological, respiratory, and cardiovascular symptoms. Patients have reported a myriad of post-viral symptoms ranging from fatigue and depression to chest pain and shortness of breath. Given the diverse array of symptoms, establishing an accurate diagnostic criterion is essential not just for clinical practice but also for research aimed at understanding long COVID’s pathophysiology and potential treatment options.
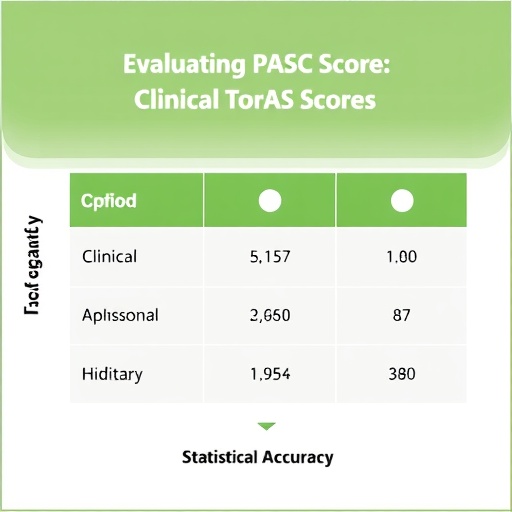
In their groundbreaking article, Azola and colleagues explore how precisely the PASC score correlates with clinical evaluations, aiming to determine whether the score can serve as a standalone diagnostic tool. The researchers executed a comparative study that involved patient assessments and extensive statistical analyses. Their findings are particularly poignant, given that many clinicians are still struggling with how best to identify and treat long COVID, a condition that defies conventional diagnostic methods.
The study involved a broad spectrum of participants, capturing a diversity of experiences with long COVID. Researchers meticulously collected data through questionnaires that assessed a variety of symptoms and their severity. This comprehensive approach would allow the authors to draw meaningful conclusions about the PASC score’s performance. By juxtaposing clinical evaluations against the PASC score, they could discern the areas where the score excels and where it might fall short.
One of the key revelations from the study was the score’s unexpected variability in accuracy among different demographics. While the PASC score may have been initially assessed as an effective diagnostic tool, the team’s findings raised questions about its universal applicability across diverse populations. Some patient cohorts displayed a significant discrepancy between their clinical symptoms and their corresponding PASC scores, thus highlighting a need for more adaptable diagnostic criteria that encompass the various manifestations of long COVID.
The implications of this research extend beyond diagnostic criteria; they touch directly on the potential for improved treatment strategies and healthcare support for those afflicted with long COVID. Accurate diagnosis is often the precursor to effective treatment. If clinicians cannot reliably identify an underlying condition, the result may be inadequate care or, worse, misdiagnosis. The risk of medical gaslighting could result in patients feeling isolated and misunderstood as they navigate their long-term recovery journeys.
Statistical accuracy is another cornerstone of this study. By engaging in rigorous analyses of the relationship between the PASC score and clinical findings, the researchers positioned their inquiry within a framework of empirical evidence. This commitment to statistic validity enhances the credibility of their conclusions, as it underscores the importance of data-driven decision-making in clinical settings. The team employs advanced statistical methodologies to scrutinize the results, accounting for variables that could influence outcomes.
One interesting finding from their analysis was the importance of patient-reported outcomes in bolstering the predictive power of the PASC score. When patients self-reported their symptoms, combined with clinical evaluations, researchers noted enhanced diagnostic accuracy. This intersection of subjective experience and objective measurement is vital; it indicates that medical professionals might achieve more precision by integrating patient narratives into their assessments.
Moreover, the study emphasizes the urgent need for further research into the underlying mechanisms of long COVID. Identifying a robust diagnostic tool, while essential, remains one part of a larger puzzle. Understanding the biological pathways that contribute to long COVID will allow researchers and clinicians to better classify syndromes and tailor treatments that address not only symptoms but also the root causes of prolonged illness.
Equally significant are the social and economic factors associated with long COVID, which the article subtly alludes to. A widespread and effective diagnostic criteria could facilitate access to necessary healthcare services, disability benefits, and social systems designed to support those unable to return to their pre-COVID lives. Thus, the importance of accurate diagnosis transcends the individual, impacting public health systems on a larger scale.
As the research community continues to grapple with the repercussions of the COVID-19 pandemic, the validation or invalidation of tools like the PASC score will significantly impact future public health strategies. Policymakers, healthcare providers, and researchers must remain vigilant in their efforts to adapt evidence-based strategies in response to evolving data and patient needs.
Ultimately, as Azola, Dastgheyb, and Easter’s study illustrates, the quest to ascertain the true efficacy of the PASC score in long COVID diagnosis embodies a larger narrative about our collective struggle against lingering COVID effects. It exemplifies the critical need for a flexible, evidence-based approach to diagnosing complex conditions to ensure that all patients receive the care and understanding they rightfully deserve.
In conclusion, the exploration of the PASC score’s clinical versus statistical accuracy provides critical insights into the evolving landscape of long COVID diagnosis. As this field progresses, the study underscores the responsibility of the medical community to prioritize accuracy, patient engagement, and ongoing research into long COVID’s etiology. This commitment will facilitate the development of effective diagnostic tools and treatments, ultimately improving the lives of countless individuals worldwide.
Subject of Research: The clinical versus statistical accuracy of the PASC score in diagnosing long COVID.
Article Title: Putting the PASC Score to the Test: Clinical vs. Statistical Accuracy in Long COVID Diagnosis.
Article References:
Azola, A., Dastgheyb, R.M., Easter, R. et al. Putting the PASC Score to the Test: Clinical vs. Statistical Accuracy in Long COVID Diagnosis.
J GEN INTERN MED (2025). https://doi.org/10.1007/s11606-025-10042-6
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s11606-025-10042-6
Keywords: Long COVID, PASC score, clinical diagnostic accuracy, statistical validity, public health.