Cerebellar mutism syndrome (CMS) is a perplexing and multifaceted condition primarily observed in pediatric populations following posterior fossa surgeries. As the medical community continues to unravel the complexities surrounding CMS, recent studies have focused on the role of preoperative imaging biomarkers in predicting the onset of this syndrome. In a groundbreaking pilot study led by Laustsen et al., researchers sought to determine the interobserver variability in assessing these imaging biomarkers. Understanding the consistency of evaluations among different observers is pivotal for developing reliable preoperative assessment protocols that can ultimately enhance patient outcomes.
The study, published in the journal Pediatric Radiology, highlights the necessity of multiobserver approaches in the interpretation of imaging data. Given that cerebellar mutism often presents as a sudden onset of mutism coupled with other neurological deficits following surgical intervention, preoperative imaging plays a crucial role in stratifying risk. The ability to accurately identify potential biomarkers for CMS could lead to enhanced surgical planning, patient counseling, and more tailored postoperative care.
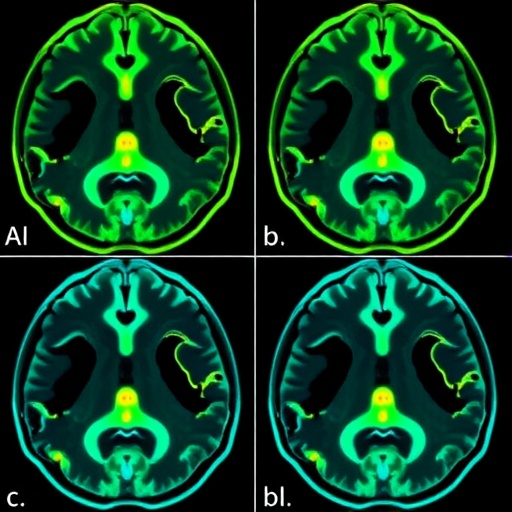
In the context of this research, the researchers assembled a cohort of radiologists and clinicians to evaluate preoperative imaging findings from a defined set of patients diagnosed with posterior fossa tumors. Each observer was tasked with assessing specific imaging biomarkers that prior studies had correlated with the incidence of CMS, including morphological and functional changes in brain structures noted on MRI. The insights gained from this multiobserver pilot study are expected not only to benefit imaging protocols but also to enhance overall multidisciplinary approaches in the management of conditions surrounding posterior fossa tumors.
The researchers documented variation in interpretations across multiple observers, revealing significant discrepancies in how imaging biomarkers were assessed. This interobserver variability poses a challenge, as it complicates the establishment of standardized diagnostic criteria necessary for effective management of CMS. The implications of these findings are profound, as they underscore the need for further training and calibration among radiologists and clinicians who interpret neuroimaging in pediatric populations.
Moreover, the study emphasized the quantitative assessment metrics required to analyze the reliability of observer assessments. By employing statistical measures such as Cohen’s kappa coefficient, the researchers could determine the degree of agreement among observers regarding the presence or absence of specific biomarkers. This rigorous evaluation served to illuminate areas where consensus was achieved and where significant variations existed, informing future refinements in imaging protocol development.
The complexity of cerebellar mutism syndrome itself is compounded by the various etiological factors and surgical techniques employed. During the surgical resection of posterior fossa tumors, alterations in cerebellar pathways can contribute to the onset of CMS. Therefore, the study posits that gaining a deeper understanding of the predictive nature of preoperative imaging biomarkers becomes even more crucial. It can guide surgical teams in making informed decisions regarding intervention strategies and anticipate possible postoperative complications.
In consideration of the growing body of literature surrounding CMS, the interobserver variability findings urge the need for collaborative efforts in developing comprehensive training programs aimed at standardizing imaging evaluations. With appropriate educational frameworks in place, the medical community can work toward minimizing discrepancies in interpretation outcomes, fostering a more reliable approach to diagnosing and managing CMS in affected pediatric patients.
In parallel, researchers are continuously investigating the biological underpinnings of cerebellar mutism syndrome. Efforts to explore the neurobiological mechanisms that may predispose certain patients to develop CMS post-surgery are essential. Identifying specific neuroanatomical correlates may not only refine the predictive value of imaging findings but also enhance our understanding of the syndrome. Such insights could pave the way for novel therapeutic interventions aimed at mitigating the cognitive and communicative deficits associated with CMS.
As the research progresses, the collaboration between radiologists, surgeons, neurologists, and neuropsychologists becomes increasingly vital. A multidisciplinary approach to CMS management will provide a holistic view of the patient’s needs, ensuring that care is not only focused on the surgical outcome but also on the long-term developmental trajectory of pediatric patients. Building partnerships among professionals who deal with different facets of CMS would facilitate a more thorough understanding of the syndrome from diagnosis through treatment and beyond.
In conclusion, the pilot study led by Laustsen et al. serves as a crucial stepping stone in the journey toward a more standardized and reliable understanding of preoperative imaging biomarkers for cerebellar mutism syndrome. By revealing the inherent interobserver variability in imaging assessments, the study opens the door for further research aimed at refining diagnostic criteria and improving the reliability of imaging practices. Enhanced consistency in how imaging biomarkers are evaluated could ultimately lead to better prognostic capabilities and more tailored interventions for young patients facing the complexities of CMS.
Through collaborative efforts focused on research, education, and clinical practice, the potential to improve outcomes for those affected by cerebellar mutism syndrome has never been more attainable. As the understanding of CMS continues to evolve, it is imperative that medical professionals unite in their efforts toward advancing knowledge and care for this challenging condition.
Subject of Research: Interobserver variability in assessing preoperative imaging biomarkers for cerebellar mutism syndrome.
Article Title: Interobserver variability in assessing preoperative imaging biomarkers for cerebellar mutism syndrome: a multiobserver pilot study.
Article References: Laustsen, A., Dineen, R., Ilginiene, J. et al. Interobserver variability in assessing preoperative imaging biomarkers for cerebellar mutism syndrome: a multiobserver pilot study. Pediatr Radiol (2025). https://doi.org/10.1007/s00247-025-06326-y
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s00247-025-06326-y
Keywords: Cerebellar mutism syndrome, preoperative imaging, interobserver variability, pediatric radiology, biomarkers, posterior fossa tumors, multidisciplinary approach.