In a groundbreaking study, researchers have shed light on the nuanced and profound effects of estrogen on murine macrophages, revealing distinctive sex differences that could carry significant implications for future biomedical research and therapies. The study, conducted by a team led by Veintimilla et al., has demonstrated that various cell lines respond differently to estrogen, an insight that challenges long-held assumptions about sex-based hormonal influences in immune cell function.
Macrophages, a type of white blood cell, play a crucial role in the immune system’s defense against pathogens and are key players in inflammation and tissue repair. Traditionally, studies have often used a one-size-fits-all approach to understand the immune response, largely ignoring the potential variations by sex. The current research emphasizes that these differences are not merely anecdotal; rather, they point to profound biological mechanisms that inform our understanding of immune responses.
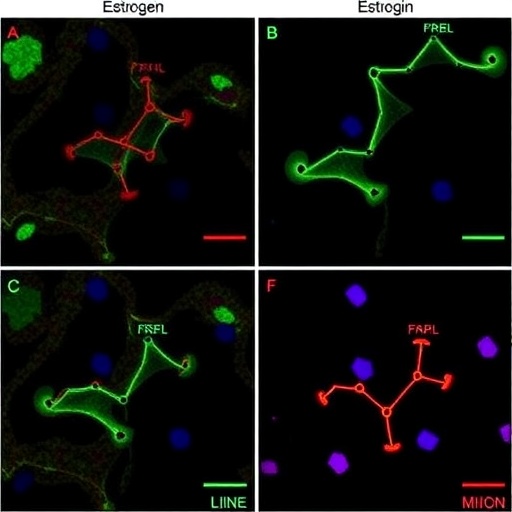
One primary finding of the study is that the response of macrophages to estrogen is not only cell line-specific but directly correlates with the sex of the organism from which these cells are derived. This challenges the prevailing notion that macrophage functions are uniform across sexes, urging scientists to reconsider experimental designs and therapeutic strategies that often overlook these vital distinctions. For instance, the researchers observed that estrogen exposure led to differential expression of cytokines, which are critical signaling molecules in immune responses, showcasing a variably robust response between male and female macrophages.
The significance of these findings cannot be overstated, especially when considering the increasing recognition of sex as a biological variable in medical research. Historically, the majority of biomedical studies have predominantly used male subjects, which can bias results and lead to a skewed understanding of how diseases manifest and respond to treatments in diverse populations. This new perspective encourages a re-evaluation of previous research, advocating for a more comprehensive inclusion of female subjects in studies, particularly in immunology and pharmacology.
Additionally, the research showcases the complexity of estrogen’s role within the immune system. Estrogen has been known to have immunomodulatory effects, but the specifics of these effects—how they vary by cell type and sex—remain poorly understood. By providing clear evidence of these variations, the study opens the door for innovative research directions aimed at understanding how estradiol and its metabolites impact macrophage function and, consequently, the overall immune response.
In practical terms, these insights could lead to more effective, sex-specific approaches in developing therapeutic interventions for autoimmune diseases, cancer, and other conditions where macrophages play a key role. For instance, drugs that leverage the immune-modulating effects of estrogen might be tailored differently for male and female patients, enhancing efficacy and minimizing adverse effects. Such advancements could represent a paradigm shift in how therapies are constructed, administered, and monitored in clinical settings.
Moreover, this research has broader implications for understanding sex differences in susceptibility to various diseases. For instance, women often have a higher prevalence of certain autoimmune diseases, and this study provides a plausible biological basis for these observations. It reinforces the idea that biology, particularly hormonal influences, affects disease susceptibility and progression, suggesting that sex-specific diagnostics and therapeutics could greatly enhance patient outcomes.
The interplay between hormone levels and immune function also raises questions about the role of environmental and lifestyle factors in modulating these responses. The authors point out that factors such as diet, stress, and exposure to endocrine-disrupting chemicals can significantly influence estrogen levels and, by extension, the immune response. This emphasizes the importance of a holistic approach in understanding health and disease, where lifestyle interventions could complement traditional medical treatments.
Moving forward, the study sets the stage for further investigations into other immune cells and their responses to estrogens. It highlights the necessity of dissecting these mechanisms to fully elucidate the underpinning biology of immune responses in varying contexts. By expanding the focus beyond macrophages, researchers may uncover additional sex differences that influence how various immune cells behave under hormonal influence.
Furthermore, this pivotal work underscores the importance of multi-disciplinary collaboration among immunologists, endocrinologists, and gender studies experts. The convergence of these fields is essential for effectively addressing the complexities of sex differences in health and disease, paving the way for integrative strategies that respect and utilize these differences.
As awareness and understanding of sex as a biological variable grow, future research endeavors must capitalize on this momentum. It is imperative that the scientific community not only integrates sex-specific analyses in immune research but also advocates for policy changes in research funding and experimental guidelines that prioritize these dimensions. Such changes could help dismantle the historical biases that have persisted in biomedical research and potentially lead to a new era of personalized medicine.
In summary, the revelations presented by Veintimilla et al. mark an important leap forward in our understanding of estrogen’s effects on macrophages and open up vital pathways for research, treatment development, and health policy reform. Embracing the intricate relationship between sex and biology could revolutionize our approach to health science, ensuring that treatments are as effective and inclusive as possible.
As researchers continue to delve into these critical questions, the implications of their findings will undoubtedly permeate through disciplines, providing a rich terrain for future investigations aimed at improving health outcomes for all individuals, irrespective of sex.
Subject of Research: The specific effects of estrogen on murine macrophages and the functional sex differences observed in immune responses.
Article Title: Cell line-specific estrogen responses uncover functional sex differences in murine macrophages.
Article References: Veintimilla, A.M., Turner, Z., Owusu-Boaitey, N. et al. Cell line-specific estrogen responses uncover functional sex differences in murine macrophages. Biol Sex Differ 16, 75 (2025). https://doi.org/10.1186/s13293-025-00760-1
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s13293-025-00760-1
Keywords: Estrogen, macrophages, sex differences, immune response, biomedical research, cytokines, personalized medicine, autoimmune diseases.