Title: Enhancing Chronic Care: The Importance of Teamwork in Primary Care Settings
In the realm of healthcare management, the significance of regular follow-up visits cannot be understated, especially for patients managing chronic conditions. Recent research has shed light on the varying levels of success among primary care clinics in achieving consistent visit regularity for this patient population. A study aimed at identifying the strategies employed by high-performing clinics reveals crucial insights into how collaborative efforts and teamwork can optimize care delivery.
The background of the study begins with the recognition that chronic conditions necessitate ongoing management and monitoring. While many clinics make efforts to encourage patient follow-up visits, not all achieve similar levels of success. This inconsistency raises questions about the underlying factors that contribute to effective patient engagement and retention in follow-up care. By examining clinics distinguished by their temporal regularity—the frequency at which patients attend follow-ups—researchers sought to uncover the best practices that lead to positive outcomes.
To gather comprehensive data, the study employed a qualitative approach, using semi-structured interviews with a diverse group of healthcare professionals. Participants included 15 primary care physicians, 12 nurses, 15 administrative staff, and 4 pharmacists from 12 different clinics. The selection of clinics was intentional, showcasing a balanced representation of those with high and low rates of follow-up visit attendance. This methodology allowed for a nuanced exploration of the inner workings of primary care teams and their strategies to foster patient adherence to scheduled appointments.
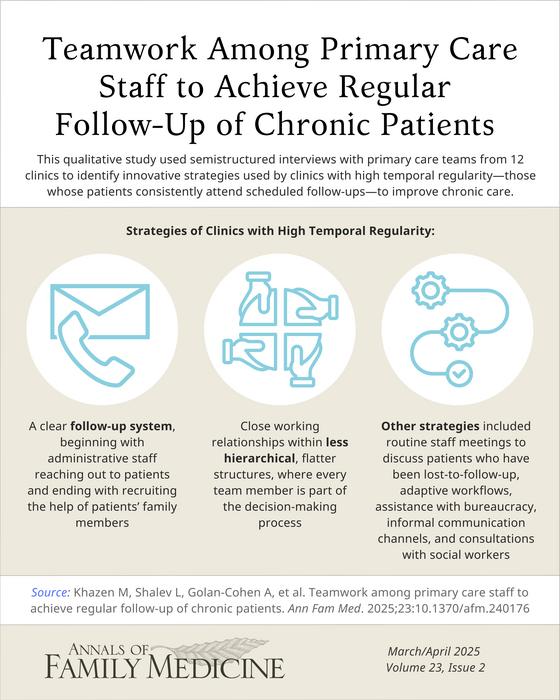
The results of the study revealed a set of key differentiators that set high-temporal regularity clinics apart from those struggling with patient follow-ups. Foremost among these was the emphasis on teamwork and collaboration among staff members. Clinics that reported success in follow-up attendance showcased less hierarchical structures, where all team members—administrative staff, nurses, and physicians alike—were actively involved in decision-making processes. This approach not only improved communication within teams but also cultivated a sense of shared responsibility for patient outcomes.
Another significant finding highlighted the importance of structured follow-up systems, particularly regarding patients who miss appointments. High-performing clinics implemented systematic approaches to manage "no-show" patients, beginning with administrative staff reaching out to these individuals shortly after their missed appointments. This proactive outreach often involved collaborating with patients’ family members to encourage their participation and support in securing follow-up visits. Such innovative strategies not only impacted attendance rates but also demonstrated a commitment to patient-centered care.
Additionally, the study showcased a range of unique tactics employed by high-temporal regularity clinics to enhance their engagement with patients. Routine staff meetings provided a platform for team members to discuss challenges, share successes, and strategize on improving care processes. Adaptive workflows allowed for flexibility in responding to patient needs and fostering a more efficient clinic environment. Moreover, staff members employed informal communication channels to keep everyone updated on patient statuses and follow-up requirements, further solidifying their collaborative efforts.
Patients themselves can be impacted by the degree of teamwork exhibited in their care. The study found that clinics emphasizing interdisciplinary collaboration experienced better patient engagement. Incorporating professionals from various backgrounds—such as social workers—into the care team enabled a holistic view of patient needs. This not only improved access to resources but also enhanced trust and communication between patients and their healthcare providers.
In light of these findings, the implications for practice are substantial. Healthcare providers and administrators can leverage the insights from this research to develop strategies aimed at improving follow-up visit regularity for chronic patients. Building a culture of teamwork and collaboration within primary care settings can lead to better patient outcomes, decreased healthcare costs, and a more efficient use of healthcare resources. Furthermore, adopting innovative practices and focusing on patient engagement can transform the standard of care provided.
In conclusion, the study’s exploration of teamwork among primary care staff illuminates the path toward optimizing chronic care management. By embracing structured follow-up systems, proactive outreach, and interdisciplinary collaboration, clinics can significantly enhance their performance in maintaining regular patient visit attendance. This research not only contributes valuable knowledge to the field of healthcare but also serves as a call to action for primary care facilities to cultivate teamwork as a cornerstone of effective chronic disease management.
Subject of Research: Strategies to Improve Follow-Up Visits for Chronic Patients in Primary Care
Article Title: Enhancing Chronic Care: The Importance of Teamwork in Primary Care Settings
News Publication Date: 24-Mar-2025
Web References: Annals of Family Medicine
References: Not specified
Image Credits: Credit: Annals of Family Medicine
Keywords: Chronic care, follow-up visits, teamwork, primary care, patient engagement, healthcare management.