In a groundbreaking study set to reshape our understanding of substance use disorder treatment among women, researchers from Columbia University’s Mailman School of Public Health have unveiled compelling evidence that enrollment in Medicaid, when combined with other government assistance programs, markedly increases treatment uptake for drug use disorder (DUD) and opioid use disorder (OUD). This discovery, published in the American Journal of Preventive Medicine, elucidates the intricate interplay between healthcare access and social support mechanisms, emphasizing a holistic approach to overcoming persistent barriers that have clouded treatment disparities for decades.
The research addresses a critical public health challenge: why do significant gaps in treatment access persist among women grappling with substance use disorders, despite advances in medication-assisted therapies? By leveraging data from the 2022 National Survey on Drug Use and Health (NSDUH), the investigators analyzed responses from nearly 3,000 women aged 18 to 64 who met criteria for past-year DUD, including a subset diagnosed with OUD. The methodological rigor incorporated adjustment for key sociodemographic confounders such as age, race/ethnicity, education, employment, marital status, and childcare responsibilities, ensuring robustness of the findings across diverse populations.
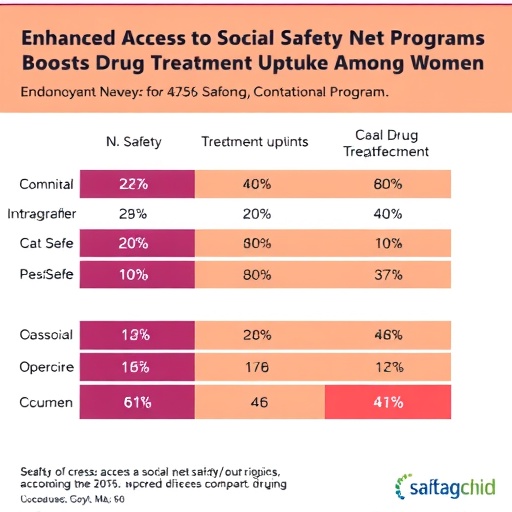
At the core of the study is the revelation that Medicaid coverage alone facilitates drug treatment access, but the coalescence of multiple social safety net programs significantly amplifies this effect. Women simultaneously receiving Medicaid and supplemental benefits—such as childcare support, SNAP nutritional aid, and employment services—exhibited substantially higher rates of treatment engagement and medication for opioid use disorder (MOUD). This confluence of support functions as a multifaceted intervention, dismantling structural impediments like the financial burden of healthcare, caregiving demands, and occupational instability that frequently impede sustained treatment adherence.
Despite these encouraging trends, the study underscores that treatment gaps remain daunting. Disturbingly, fewer than one in six women reported receiving any drug-related treatment in the past year, and only a fraction of women diagnosed with OUD—approximately 14%—accessed MOUD. This stark contrast with the 23% treatment rate observed in men spotlights an enduring gender disparity that warrants urgent policy focus and gender-sensitive intervention frameworks. The findings suggest that conventional healthcare systems must evolve beyond insurance coverage to address the social determinants intricately linked to treatment access and retention.
The investigators also illuminated the positive impact of standalone government assistance programs in the absence of Medicaid. Receipt of any form of public aid independently correlated with higher odds of treatment, suggesting that these services can serve as critical conduits for engaging vulnerable populations. The implications are clear: expanding and integrating social services with healthcare delivery could forge new pathways to care that transcend traditional clinical settings.
Crucially, the study advocates for comprehensive policy reforms that incorporate treatment referrals within the spectrum of social support benefits. Integrating housing assistance, transportation solutions, vocational training, and childcare provisions into treatment paradigms could mitigate the multifactorial barriers faced by women with substance use disorders. The researchers posit that such targeted, multidimensional interventions hold promise for elevating treatment engagement rates, fostering equity, and ultimately improving health outcomes.
The granular analysis conducted by lead author Sam D. Gardner and co-authors—including experts affiliated with Columbia and UCSF—demonstrates the power of large-scale epidemiological surveys combined with sophisticated statistical modeling. By stratifying participants based on the quantity and type of assistance programs accessed, the team revealed nuanced gradients of treatment likelihood, underscoring the heterogeneity within this population. This level of detail advances the scientific discourse on intersectionality in health services utilization among marginalized groups.
Underlying the study is a recognition that substance use disorder continues to exact a disproportionate toll on women, shaped by intersecting factors such as caregiving responsibilities, socioeconomic precarity, stigma, and healthcare disparities. The nuanced understanding cultivated here disrupts monolithic approaches that prioritize medical treatment alone, instead championing a paradigm that spotlights systemic and structural determinants.
Moreover, the study was supported by multiple NIH-NIDA grants and the NIH HEAL Initiative, framing it within a broader national effort to tackle opioid and substance use crises through innovative research and translational goals. The institutional backing underscores the urgency with which these findings should be operationalized in public health strategy and healthcare policy.
As medicine advances in its pharmacological arsenal against opioid dependence, research like this reminds us that access, engagement, and retention hinge on addressing life realities beyond the clinic. Future investigations will be tasked with experimentally determining how integrated social and healthcare interventions perform in real-world settings, an exigent step toward policy prescriptions that can close entrenched gender and socioeconomic treatment gaps.
In sum, this landmark study illuminates the powerful synergy between Medicaid and ancillary social support services in transforming the landscape of drug treatment among women. It calls for a recalibration of health policy that embraces comprehensive, layered interventions as vital levers to overcome the entrenched barriers to care that disproportionately burden women struggling with substance use disorders.
Subject of Research: The association between enrollment in Medicaid combined with other social safety net programs and increased receipt of drug treatment and medication for opioid use disorder among women with substance use disorders.
Article Title: Social safety net programs: the relationship with drug treatment among women
News Publication Date: June 17, 2025
Web References:
References: NIH-NIDA grants R01DA059376, T32DA031099, R36DA061635, K01DA045224 and R01DA055606; NIH HEAL Initiative
Keywords: Health and medicine