In a groundbreaking advance poised to shift the paradigm of cancer therapy management, researchers have unveiled compelling evidence that empagliflozin, a drug primarily used to treat type 2 diabetes, holds remarkable potential in protecting the liver from the damaging side effects of doxorubicin, a widely utilized chemotherapeutic agent. This discovery emerges from rigorous preclinical studies conducted on male NMRI mice, elucidating a multifaceted mechanism through which empagliflozin ameliorates hepatotoxicity induced by doxorubicin. The findings resonate with fresh hope for oncological patients who face the dual battle against cancer and the collateral organ toxicity associated with chemotherapy.
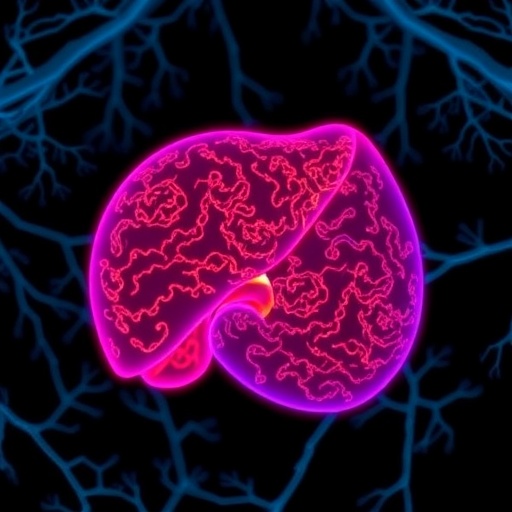
Doxorubicin has long been a cornerstone in the treatment protocols for various malignancies, revered for its potent antitumor effects. However, its clinical utility is substantially hampered by its notorious side effects, particularly hepatotoxicity, which is marked by oxidative stress, inflammation, and programmed cell death (apoptosis) within liver tissues. These adverse effects not only diminish patients’ quality of life but also limit the feasible dosage of doxorubicin, often compelling oncologists to seek compromised therapeutic regimens. The study conducted by Asgari and Kalhori decisively addresses this obstacle by investigating empagliflozin’s hepatoprotective properties and delineating the underlying biochemical pathways involved.
Empagliflozin, a selective sodium-glucose cotransporter 2 (SGLT2) inhibitor, has been predominantly employed in managing hyperglycemia through its action on renal glucose reabsorption. Intriguingly, recent insights have revealed its pleiotropic effects beyond glucose regulation, including anti-inflammatory and antioxidative properties, which prompted researchers to explore its potential in mitigating chemotherapy-induced organ toxicity. This study is seminal in revealing how empagliflozin’s pharmacological profile interacts with hepatic cellular mechanisms to counteract the deleterious oxidative and inflammatory cascades initiated by doxorubicin.
At the molecular level, doxorubicin generates excessive reactive oxygen species (ROS) within hepatocytes, precipitating oxidative stress and consequent lipid peroxidation, mitochondrial dysfunction, and activation of apoptotic pathways. The investigators discovered that empagliflozin significantly reduced markers of oxidative damage, indicating an enhancement of intrinsic antioxidant defenses in the liver. This effect likely involves the modulation of nuclear factor erythroid 2–related factor 2 (Nrf2), a master regulator of cellular antioxidant response, which empagliflozin may potentiate to restore redox homeostasis disrupted by doxorubicin.
Inflammation is another pivotal contributor to doxorubicin’s hepatotoxic profile. The drug promotes upregulation of proinflammatory cytokines such as TNF-α, IL-6, and IL-1β, which exacerbate tissue injury and propagate a damaging feedback loop. Empagliflozin was observed to markedly suppress these inflammatory mediators, signifying its role in tempering the immune response within the liver’s microenvironment. This anti-inflammatory action not only curbs immediate hepatocyte damage but may also prevent the progression to chronic liver conditions often associated with chemotherapy.
The apoptotic cell death initiated by doxorubicin is chiefly mediated through intrinsic mitochondrial pathways, characterized by the imbalance of pro- and anti-apoptotic proteins, leading to the activation of caspases and subsequent cell dismantling. The study’s findings show that empagliflozin administration preserves the expression of Bcl-2, an anti-apoptotic protein, while downregulating Bax and caspase-3 activity, effectively hindering the apoptotic cascade. This preservation of hepatocyte viability is critical for maintaining liver function during aggressive cancer treatments.
This multifactorial intervention displayed by empagliflozin not only attenuates biochemical signs of liver injury but also translates into improved histopathological outcomes. Liver tissue samples from treated mice exhibited markedly reduced necrosis, cellular swelling, and inflammatory infiltration compared to those receiving doxorubicin alone. Such histological evidence consolidates the biochemical data, painting a comprehensive picture of empagliflozin’s protective efficacy.
The employment of the NMRI male mouse model provides a robust and reproducible system for examining chemotherapeutic toxicity and therapeutic interventions, given the physiological and metabolic resemblance of their hepatic responses to humans. The relevance of these findings gains additional strength from the clinical familiarity and safety profile of empagliflozin in human subjects, underscoring the translational potential of the research.
Moreover, the study prompts a broader reconsideration of the role of SGLT2 inhibitors in oncology, potentially expanding their application beyond glycemic control to become adjunctive agents in cancer treatment regimens. This repositioning of empagliflozin could pioneer a new category of therapeutics focused on minimizing host toxicity while maximizing anticancer efficacy.
However, translating these promising preclinical results into clinical practice necessitates further rigorous trials to determine optimal dosing, timing, and safety among diverse patient populations. The hepatoprotective effect observed here may also inspire exploration into empagliflozin’s capacity to shield other organs vulnerable to chemotherapy-induced damage, such as the heart and kidneys, particularly given doxorubicin’s well-documented cardiotoxicity.
The implications of this research are immense, offering a beacon of hope for improving patient outcomes by mitigating one of the most challenging obstacles in cancer pharmacotherapy—organ toxicity. Patients undergoing doxorubicin treatment frequently endure debilitating side effects that can limit therapeutic adherence and efficacy; adjunctive therapies like empagliflozin may alleviate this burden and enhance quality of life.
Furthermore, this insight dovetails with a growing recognition of the importance of adjunctive treatments that focus not solely on tumor eradication but also on preserving and protecting the patient’s physiological integrity during rigorous cancer treatment courses. The dual action of empagliflozin—anti-inflammatory and antioxidative—positions it uniquely within this therapeutic niche.
The study conducted by Asgari and Kalhori contributes a pivotal piece to the intricate puzzle of safe and effective cancer therapy, highlighting an innovative strategy to circumvent the adverse effects of chemotherapeutics. This intersection between diabetes medication and oncology represents a fertile frontier for scientific inquiry and clinical innovation.
As the scientific and medical communities await further validation through clinical trials, empagliflozin’s potential as a hepatoprotective agent could redefine current standards of care and foster the development of more holistic, patient-centered oncological treatment frameworks that integrate organ protection with tumor control.
In essence, the revelation of empagliflozin’s protective capacities against doxorubicin-induced liver injury is a significant stride toward more tolerable and effective cancer therapies. It exemplifies the power of interdisciplinary research and drug repurposing in overcoming longstanding therapeutic challenges and advancing patient care.
Subject of Research: Investigation of empagliflozin’s protective effects against doxorubicin-induced hepatotoxicity in male NMRI mice.
Article Title: Empagliflozin mitigates doxorubicin-induced hepatotoxicity by reducing inflammation, oxidative stress, and apoptosis in male NMRI mice.
Article References:
Asgari, N., Kalhori, Z. Empagliflozin mitigates doxorubicin-induced hepatotoxicity by reducing inflammation, oxidative stress, and apoptosis in male NMRI mice. Med Oncol 42, 542 (2025). https://doi.org/10.1007/s12032-025-03113-5
Image Credits: AI Generated