Recent research has provided compelling insights into the relationship between dietary habits and childhood asthma, a condition affecting millions of children worldwide. A study led by Xue et al., which utilized the robust NHANES dataset, explored how various dietary indices correlate with the prevalence of asthma in children. This groundbreaking research not only highlights the importance of nutrition in respiratory health but also introduces visceral adiposity indicators as potential mediators in this association.
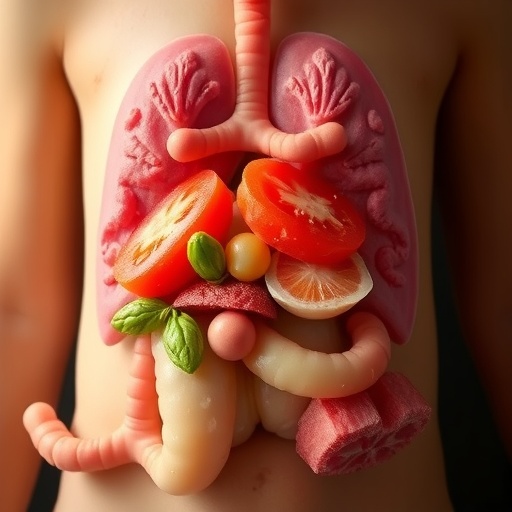
The investigation into dietary indices aimed to analyze the dietary patterns such as overall dietary quality, macronutrient compositions, and food group consumption. This multifaceted approach emphasized the significance of diverse dietary components, revealing that certain diets could play a protective role against the development of childhood asthma. Each dietary index encompassed different elements, ranging from the Mediterranean diet rich in fruits, vegetables, and healthy fats, to Western dietary patterns characterized by high processed foods, which may exacerbate respiratory issues.
Furthermore, the study collected data from NHANES, a comprehensive source that assesses the health and nutritional status of adults and children in the United States. NHANES provides valuable insights through its dietary recalls, which assist researchers in establishing clear links between nutrition and health outcomes. The use of a nationally representative sample in assessing dietary habits brings a level of credibility to the study, positioning it as a vital resource for both researchers and policymakers who are focused on pediatric health.
Visceral adiposity, commonly referred to as abdominal fat, is known to have a direct impact on inflammation and respiratory function. Xue et al. argue that this fat can produce inflammatory cytokines that exacerbate asthma symptoms and may contribute to worsening lung function. The mediating role of visceral fat in the association between dietary habits and asthma prevalence emphasizes the complexity of childhood obesity and its related health ramifications. As childhood obesity rates continue to rise, understanding its connection to respiratory diseases like asthma becomes increasingly crucial.
The researchers highlighted that not just obesity, but specifically visceral adiposity correlates with asthma incidence. This refinement in understanding allows physicians and health experts to target interventions that not only focus on asthma management but also address dietary patterns and obesity prevention from a dual perspective. The evidence presented strengthens the case for dietary interventions as a means to diminish the incidence of asthma in children, aligning nutritional education with public health initiatives.
Another critical component of this research is how specific dietary patterns can be modified to improve child health outcomes. Much of the evidence suggests that a shift away from refined sugars and high-fat, processed foods can positively affect digestive health. These changes undoubtedly influence visceral fat accumulation and related inflammation, indicating a potential pathway for reducing asthma risk. Xue et al.’s work encourages stakeholders to advocate for healthy eating amongst children, combining this with public health initiatives aimed at reducing asthma prevalence.
The article underscores the essential role that parents, educators, and healthcare providers play in regulating children’s dietary intake. Empowering families with knowledge about healthy eating habits can potentially transform the landscape of childhood health. In a world increasingly dominated by convenience foods, this research calls for innovative strategies to make wholesome food more accessible and appealing to young children and their families.
Furthermore, another fascinating outcome of this study is its relevance to future research directions. As researchers investigate the links between dietary indices and respiratory health, there is an opportunity to explore how socioeconomic factors influence access to nutritious foods. Understanding these disparities is vital, as they also significantly contribute to health inequalities experienced by children living in low-income households.
Additionally, the study raised pertinent questions regarding the generalizability of its findings across diverse populations. Nutrition is highly contextual, influenced by cultural practices, food availability, and economic circumstances. Future investigations could expand on this research by analyzing different demographics, including various age groups, ethnic backgrounds, and geographic locations. This would provide a more comprehensive understanding of dietary impacts on asthma in a multicultural society.
Furthermore, this study illuminates the potential for policy change at a systemic level. As the relationship between diet, obesity, and asthma becomes clearer, practitioners and policymakers may prioritize nutritional interventions in schools and community programs aimed at preventing childhood asthma. Consequently, the findings may catalyze changes in existing policies that influence food marketing to children, school lunch programs, and public health campaigns.
In conclusion, Xue et al.’s research advances the dialogue surrounding childhood asthma and emphasizes an important cultural shift toward understanding the holistic influences of diet on health. The work encourages a multidisciplinary approach that brings together nutritionists, public health experts, and healthcare providers to unite against the escalating rates of childhood asthma and related diseases. Through these concerted efforts, a healthier future can be forged for the next generation.
In light of these findings, the study not only makes significant contributions to the existing body of literature but raises the bar for future inquiries into dietary practices and their larger implications for child health. As researchers continue to explore these intersections, the hope is for more proactive measures to emerge, leading to both improved nutritional habits and diminished prevalence of respiratory illnesses among children.
Subject of Research: Dietary indices and childhood asthma
Article Title: Association between five dietary indices and childhood asthma: the mediating role of visceral adiposity indicators using NHANES data.
Article References:
Xue, Nc., Xu, Zh., Gao, Y. et al. Association between five dietary indices and childhood asthma: the mediating role of visceral adiposity indicators using NHANES data.
BMC Pediatr 25, 937 (2025). https://doi.org/10.1186/s12887-025-06233-z
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s12887-025-06233-z
Keywords: Childhood asthma, dietary habits, visceral adiposity, NHANES data, public health, nutrition.