Invasive lung adenocarcinoma (LUAD) continues to represent a significant challenge in oncology, primarily due to its aggressive nature and the complexities involved in its prognosis. A critical pathological feature influencing patient outcomes is lymphovascular invasion (LVI), wherein cancer cells infiltrate lymphatic and vascular structures, facilitating metastasis and ultimately worsening the clinical prognosis. Traditionally, the accurate prediction of LVI before surgery has been hindered by limitations in imaging modalities, creating a pressing need for innovative, non-invasive diagnostic tools that can enhance clinical decision-making.
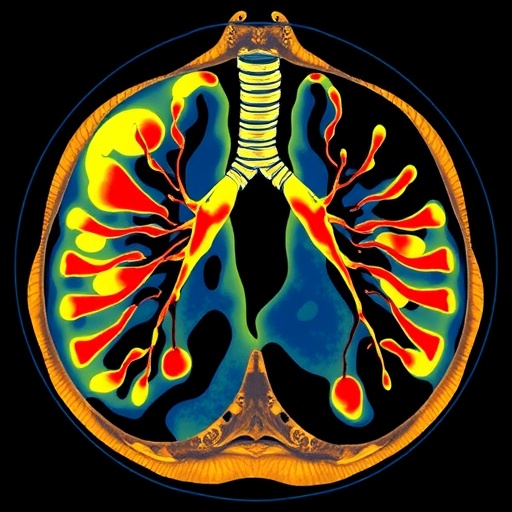
Recent advances in the field of radiomics—the comprehensive extraction of quantitative features from medical images—offer promising avenues to overcome these challenges. By harnessing high-throughput data derived from computed tomography (CT) scans, radiomics can reveal subtle imaging biomarkers that are often imperceptible to the human eye. These biomarkers, when combined with clinical indicators, may enable more precise and personalized predictions regarding LVI status in patients with invasive LUAD.
A pioneering study published in BMC Cancer has explored the integration of intratumoral and peritumoral CT radiomics features to develop predictive models for LVI in LUAD patients. The investigators analyzed CT images from a cohort of over 600 patients across two institutions, extracting an extensive array of more than 1,200 quantitative radiomic features from distinct tumor regions. This comprehensive approach allowed for a detailed morphological and textural characterization of both the tumor bulk and its surrounding microenvironment, which is critically implicated in tumor invasion dynamics.
The research team divided their patient population into training, internal, and external validation cohorts, enabling robust assessment of the model’s generalizability across diverse clinical settings. Utilizing advanced machine learning techniques, they constructed three distinct radiomics models: one focusing on the gross tumor alone, a second encompassing both gross tumor and peritumoral regions, and a third analyzing the peritumoral area in isolation. These models were evaluated based on their ability to discriminate LVI presence, measured through the area under the receiver operating characteristic curve (AUC).
Among the three approaches, the model incorporating both intratumoral and peritumoral features demonstrated superior predictive performance. This combined gross tumor and peritumoral (GPT) model revealed AUC values of 0.83 in the training set and maintained robust prediction capabilities with AUCs of 0.79 and 0.75 in internal and external validation sets, respectively. These findings underscore the clinical value of assessing not only the tumor itself but also its interface with the surrounding tissue, a region known to harbor critical biological interactions facilitating vascular and lymphatic spread.
In parallel, the study also identified key clinical parameters independently associated with LVI through rigorous statistical analysis. The preoperative carcinoembryonic antigen (CEA) level, tumor diameter, and the presence of spiculation on CT scans emerged as significant predictors. Incorporating these clinical indicators alongside the radiomic signature resulted in a composite predictive model with further enhanced accuracy. The integrated model yielded AUCs of 0.84, 0.82, and 0.77 across the training, internal, and external cohorts, respectively, outperforming models based solely on imaging or clinical data.
This multifaceted approach highlighting the synergy between image-derived radiomic features and conventional clinical factors represents a substantial step forward in the non-invasive preoperative assessment of LUAD. From a clinical perspective, the ability to predict LVI status before surgical intervention could enable thoracic oncologists to stratify patients according to risk, personalize therapeutic regimens, and potentially improve survival outcomes by identifying those who may benefit from more aggressive treatments or closer postoperative surveillance.
The methodology employed in this study involved comprehensive feature extraction from high-resolution CT images, capturing a spectrum of matrix-based texture descriptors and wavelet transformations, which provide deep insights into tumor heterogeneity. Radiomic features related to shape, intensity, and texture likely reflect the complex biological processes underpinning tumor growth and vascular invasion, offering a quantitative surrogate marker unattainable through standard radiological interpretation.
Furthermore, the inclusion of peritumoral radiomics is especially notable, as the tumor microenvironment plays a pivotal role in facilitating cancer progression and metastasis. By extending analysis beyond the tumor boundaries, the researchers tapped into spatial patterns of tissue alterations adjacent to the tumor that may signal early invasion of lymphovascular structures. These pioneering insights highlight the necessity of looking beyond conventional tumor metrics to fully characterize malignant potential.
The clinical applicability of such predictive models holds profound implications for advancing precision medicine in lung cancer care. As lung adenocarcinoma comprises a heterogeneous group of tumors with variable behavior, preoperative LVI prediction via non-invasive imaging biomarkers could inform decisions surrounding surgical resection margins, lymph node dissection extent, and the necessity for neoadjuvant therapies. This stratification may ultimately reduce overtreatment and associated morbidities while ensuring optimal oncologic control for high-risk patients.
Moreover, the study sets a precedent for the integration of big data analytics, artificial intelligence, and clinical oncology, showcasing a translational framework whereby computational tools augment physician capabilities. Radiomics, when validated in large multicenter cohorts as exemplified in this investigation, can become an indispensable component of the oncologic diagnostic arsenal, fostering more nuanced risk assessments and guiding tailored interventions.
Despite the encouraging results, certain challenges remain for the widespread clinical implementation of radiomics models. Standardization of imaging protocols, reproducibility of feature extraction algorithms, and prospective validation in randomized clinical trials are necessary to cement the role of radiomics as a standard diagnostic tool. Additionally, interdisciplinary collaboration among radiologists, oncologists, bioinformaticians, and machine learning experts will be critical to overcome technical and methodological hurdles.
Looking ahead, the integration of radiomics with emerging molecular and genomic biomarkers could further enhance prediction accuracy and provide a holistic view of tumor biology. Combining imaging phenotypes with genetic profiles may unravel novel mechanisms underlying lymphovascular invasion and identify new therapeutic targets. This multimodal approach embodies the future of oncology, leveraging the convergence of data science and molecular medicine.
In conclusion, this innovative study provides compelling evidence that CT radiomics models incorporating intratumoral and peritumoral features, combined with key clinical parameters, offer a powerful non-invasive method for predicting lymphovascular invasion in invasive lung adenocarcinoma. By facilitating early identification of patients at higher risk for poor prognosis, this approach promises to refine risk stratification, tailor treatment strategies, and ultimately improve clinical outcomes. The findings underscore the transformative potential of radiomics in lung cancer management and highlight the importance of ongoing research bridging advanced imaging analytics with pragmatic clinical applications.
Subject of Research: Non-invasive prediction of lymphovascular invasion in invasive lung adenocarcinoma using intratumoral and peritumoral CT radiomics combined with clinical indicators
Article Title: The clinical value of predicting lymphovascular invasion in patients with invasive lung adenocarcinoma based on the intratumoral and peritumoral CT radiomics models
Article References:
Lin, M., Zhao, C., Huang, H. et al. The clinical value of predicting lymphovascular invasion in patients with invasive lung adenocarcinoma based on the intratumoral and peritumoral CT radiomics models. BMC Cancer 25, 1752 (2025). https://doi.org/10.1186/s12885-025-15128-2
Image Credits: Scienmag.com
DOI: 10.1186/s12885-025-15128-2 (Published 12 November 2025)