A groundbreaking advancement in liver tissue engineering has emerged from researchers at Tsinghua University, unveiling a novel human liver organoid platform that authentically replicates the liver’s intricate metabolic zonation. This innovative platform offers unprecedented opportunities for elucidating liver disease mechanisms and enhancing preclinical drug screening, addressing a long-standing challenge in recapitulating the liver’s spatial functional diversity in vitro.
The liver’s unique architecture is characterized by its metabolic zonation, where hepatocytes in distinct regions—the periportal (portal vein, PV) and pericentral (central vein, CV) zones—exhibit specialized functions directed by region-specific signaling pathways. Wnt/β-catenin signaling predominantly governs the pericentral region, while Notch signaling pathways drive periportal activities. These discrete signaling environments enable the liver to efficiently regulate complex metabolic, synthetic, and detoxification processes that are vital for systemic homeostasis.
Leveraging extensive transcriptomic analyses from both human and rodent liver tissues, the team meticulously mapped the spatial distribution of signaling pathways instrumental in liver zonation. This molecular blueprint revealed that genes associated with Wnt ligand WNT2 and Notch ligand DLL4 are expressed predominately in endothelial cells within their respective zones, forming the basis for generating engineered microenvironments. Confirmation through immunofluorescence and immunohistochemical studies on human liver sections validated these spatial patterns, providing a firm biological foundation to reconstruct zonal heterogeneity in vitro using genetically modified cell types.
Capitalizing on these insights, researchers developed two transgenic SK-Hep1 endothelial cell lines engineered to overexpress either WNT2 or DLL4. When co-cultured with primary human hepatocytes, these engineered endothelial cells orchestrated region-specific hepatocyte differentiation. The WNT2-expressing endothelial cells induced hepatocytes with enhanced cytochrome P450 enzyme activity, mimicking pericentral functions critical for xenobiotic metabolism. Conversely, DLL4-expressing cells promoted cholangiocyte-like phenotypes and enhanced bile transport characteristic of periportal zones, thereby recapitulating the spatial functional heterogeneity of the native liver.
The dynamic interplay within these organoids also enabled hepatic progenitor cells to bifurcate into hepatocyte- and cholangiocyte-dominant lineages, emulating the developmental plasticity governed by microenvironmental cues in the liver. This bifurcation is pivotal for generating organoids that not only function accurately but also reflect the liver’s developmental and regenerative biology, which has vast implications for modeling liver diseases and therapeutic interventions.
In pharmacological assays, the platform exhibited remarkable sensitivity and specificity. Upon exposure to acetaminophen, an established hepatotoxin, the WNT2 co-cultured organoids demonstrated heightened oxidative stress susceptibility coupled with a robust regenerative response upon drug withdrawal. Such findings mirror clinical hepatotoxicity and recovery patterns, positioning this organoid system as a superior model for drug-induced liver injury studies. Meanwhile, DLL4 co-cultured organoids effectively replicated cholestatic injury phenotypes, including impaired bile clearance following drug treatments, which were reversible upon administration of choleretic agents, showcasing its utility in modeling periportal pathologies.
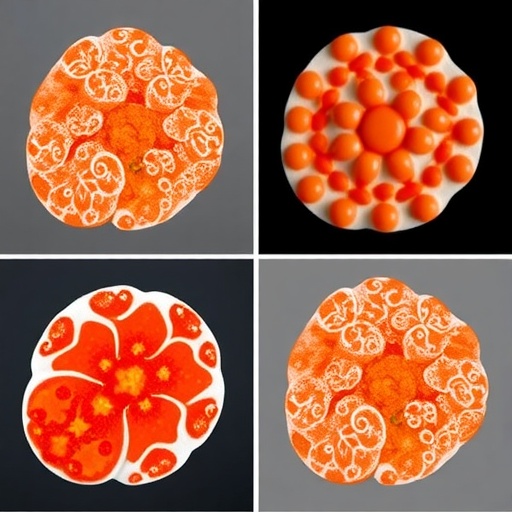
Further pushing the envelope, the team harnessed state-of-the-art 3D bioprinting technology to spatially arrange endothelial and parenchymal cells into a biomimetic liver lobule architecture. This printed construct elegantly recapitulates the liver’s zonal organization, demonstrating region-specific expression of hallmark functional proteins such as glutamine synthetase in pericentral-mimicking zones and multidrug resistance protein 2 (MRP2) along with increased albumin and urea secretion. The 3D architecture closely mimics in vivo tissue ultrastructure and function, which is critical for accurate disease modeling and drug toxicity testing.
Intriguingly, the engineered lobule exhibited selective vulnerability akin to the native liver. The pericentral-mimicking zones showed heightened sensitivity to acetaminophen-induced injury, faithfully reproducing the hepatotoxic patterns observed clinically. This spatially resolved injury response highlights the model’s capacity to dissect zonal-specific pathophysiology, a feature that has been unattainable with conventional culture systems.
This breakthrough represents a significant leap in liver bioengineering by integrating gene-engineered endothelial microenvironment cues with sophisticated 3D bioprinting. The resultant platform stands out as a physiologically relevant, spatially complex system capable of emulating the liver’s functional heterogeneity and its nuanced injury responses. Its application promises to refine preclinical drug screening pipelines, enhancing prediction accuracy for hepatotoxicity and therapeutic efficacy.
Moreover, the platform opens avenues for personalized medicine in hepatology by enabling patient-specific modeling of liver diseases, including chronic liver conditions, metabolic disorders, and drug-induced liver injuries. Implementing such organoids in precision medicine could revolutionize how liver disease progression and treatment responses are studied and managed, reducing reliance on animal models and improving translational relevance.
The collaborative effort also emphasizes the critical role of endothelial heterogeneity in orchestrating liver function and regeneration, an often-overlooked aspect in traditional liver models. By recapitulating endothelial-mediated spatial signaling, this system affords a more faithful representation of the liver’s microenvironment, offering a valuable tool for studying vascular contributions to liver health and disease.
This pioneering work from Tsinghua University’s multidisciplinary team aligns with the cutting-edge trajectory of organoid technology, marrying genetic engineering, vascular biology, and bioprinting to recreate one of the body’s most metabolically complex organs. As such, it sets a new benchmark for organoid fidelity and functional sophistication, likely inspiring a paradigm shift in liver research methodologies.
Taken together, these innovations underscore the transformative potential of engineered organoids in research and medicine. Such platforms not only promise to expedite drug development by providing reliable human tissue surrogates but also have profound implications for regenerative therapies and the modeling of liver pathologies, ultimately propelling hepatology into a new era of precision biomedical sciences.
Subject of Research: Liver organoid development mimicking region-specific liver zonation for disease modeling and drug evaluation.
Article Title: Construction of Region-Specific Liver Organoid and Fabrication of Hierarchical Functional Liver Lobule for Liver Disease Modeling and Drug Evaluation.
Web References: http://dx.doi.org/10.1016/j.scib.2025.07.021
Image Credits: ©Science China Press
Keywords: liver organoid, metabolic zonation, Wnt signaling, Notch signaling, 3D bioprinting, hepatocyte differentiation, liver disease modeling, drug toxicity, liver microenvironment, endothelial heterogeneity, acetaminophen-induced injury, cholestasis.