The COVID-19 pandemic has caused unprecedented disruptions across global healthcare systems, but its ramifications extend far beyond the immediate impact of the virus. A recently published study by Zayar, Chotipanvithayakul, Geater, and colleagues sheds light on a critical yet underexplored consequence of the pandemic: the heightened mortality among hospitalized tuberculosis (TB) patients in Thailand. This comprehensive research, appearing in Global Health Research and Policy (2025), delves deeply into how the overwhelming hospital caseload and disease severity during the pandemic have indirectly influenced TB mortality rates, revealing a complex interplay between COVID-19-related health system strain and outcomes for other infectious diseases.
Thailand, a country that has long grappled with TB as a significant public health challenge, is particularly vulnerable to disruptions in routine healthcare delivery during crises. TB requires sustained, uninterrupted treatment and careful clinical monitoring, factors complicated by the pandemic’s pressures. The study leverages detailed hospital-level data to explore how surges in COVID-19 admissions strained resources and staff capacity, thereby compromising the quality of care available to TB patients. This analysis extends beyond surface correlations, employing sophisticated statistical models to dissect the mediating effects of hospital case load and the severity of illness on patient outcomes.
Central to the study’s findings is the concept of ‘mediating variables.’ While COVID-19’s direct effects on infection and mortality dominate much discourse, this research highlights how indirect drivers—such as hospital crowding—substantially mediate mortality risk for TB patients. By operationalizing hospital caseload as a key factor, the authors reveal that facilities overwhelmed with COVID-19 cases saw a sharp decline in available resources, including isolation rooms, diagnostic services, and critical healthcare workforce hours. Consequently, TB patients admitted during peak COVID times experienced delays in diagnosis, interruptions in medication, and less intensive monitoring, which collectively escalated mortality risks.
Another striking element of the study is its focus on patient severity at admission. The authors note that the dynamic of delayed care seeking and overwhelmed emergency departments resulted in TB patients presenting at hospital admission with more advanced disease stages. Advanced TB is notoriously harder to treat and requires more intensive, prolonged clinical management—conditions less feasible when hospitals are strained by competing demands. Thus, their model accounts for how severity exacerbated mortality, acting in tandem with hospital caseload to compound negative outcomes.
The methodology utilized in this investigation is rigorous and multifaceted. The research team analyzed a cohort of hospitalized TB patients over several years, both prior to and during the COVID-19 pandemic. They integrated patient clinical data with hospital administrative records on COVID-19 admissions to construct mediation models, using regression path analysis to estimate the indirect effects. This approach lends robustness to their conclusions, distinguishing from simpler before-and-after comparisons that might obscure underlying causal pathways.
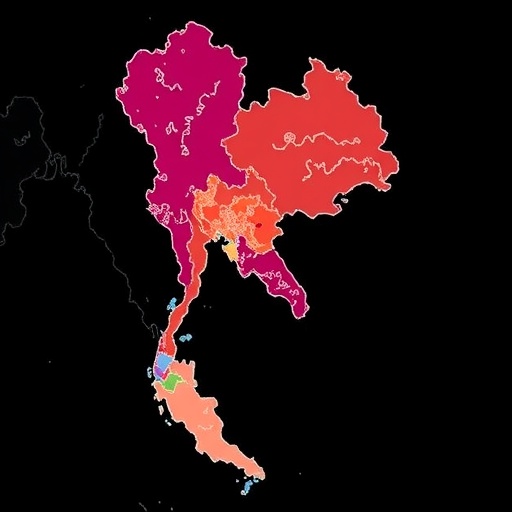
Importantly, the study also considers how regional disparities within Thailand influenced the observed patterns. Hospitals in urban areas, generally more burdened by COVID-19 caseloads, revealed more pronounced mortality increases among TB patients compared to those in rural settings. The geographic dimension reveals systemic vulnerabilities, where healthcare infrastructure differences modulate pandemic impacts on comorbid infectious diseases. Such nuanced insights are crucial for tailoring policy interventions and resource allocation during public health emergencies.
The implications of this study transcend Thailand’s borders and TB alone. It serves as a sober reminder that the ripple effects of the COVID-19 pandemic can undermine progress against other infectious diseases, especially in resource-limited contexts. International public health strategies must therefore prioritize maintaining continuity of care for diseases like TB, HIV, and malaria even amid crisis responses. Without deliberate planning and support, fragile health systems risk backsliding on hard-won gains.
From a clinical perspective, the findings recommend targeted approaches to safeguarding care standards for hospitalized TB patients during pandemics. This includes preemptive surge planning to prevent hospital overcrowding, dedicated TB wards separated from COVID-19 cohorts, and reinforcing healthcare worker capacity to manage complex co-infections. Additionally, enhancing outpatient and community-based TB services can mitigate hospital admission delays and reduce disease severity at presentation.
The study’s authors also call attention to the importance of integrating electronic health records and real-time hospital monitoring tools to better identify bottlenecks and patient care risks. Digital health innovations could play a transformative role in predicting hospital capacity thresholds, optimizing patient triage, and ensuring critical treatment continuity. In settings with limited resources, however, such technologies must be coupled with investments in training and infrastructure to realize their potential.
Moreover, the broader narrative emerging from this research underscores a fundamental lesson about health systems resilience. The COVID-19 pandemic forced rapid, often reactive adjustments in healthcare delivery, exposing gaps in coordinated care across diseases. Future pandemic preparedness efforts must embed multifunctional strategies that can simultaneously address emergent threats without sidelining endemic health burdens like TB. Strengthening health systems’ surge capacity, ensuring supply chain robustness for essential medications, and safeguarding preventive care programs should be integral priorities.
The inflow of patients with severe TB at hospital admission during the pandemic also raises questions about public health messaging and access barriers amid lockdowns and social distancing measures. Fear of COVID-19 infection or movement restrictions may have deterred patients from seeking timely care, contributing to worsened disease stages at hospitalization. Understanding these behavioral and societal dynamics is essential for designing communication campaigns that balance pandemic precautions with continued engagement in routine healthcare.
In addition to immediate clinical and system-level concerns, the study emphasizes the intersection of socio-economic factors and health outcomes during the pandemic. Thailand’s TB burden disproportionately affects marginalized populations who face greater obstacles in accessing healthcare, which may have been exacerbated by COVID-19 disruptions. Accordingly, equitable health interventions that address social determinants of health must accompany clinical efforts to reduce mortality and strengthen pandemic resilience.
Looking ahead, the need for longitudinal investigations remains paramount. This study provides a crucial empirical foundation, but ongoing surveillance and research will be critical to fully understand long-term effects on TB morbidity and mortality caused by the pandemic. As COVID-19 evolves, so too must healthcare strategies adapt to mitigate compounded risks for patients with chronic infectious diseases worldwide.
In sum, the work of Zayar and colleagues represents a vital contribution to the emerging literature on indirect effects of the COVID-19 pandemic. By focusing on the mediating roles of hospital caseload and patient severity, their research illuminates a pathway by which the pandemic has aggravated TB mortality in Thailand. This nuanced, data-driven insight should inform policymakers, clinicians, and global health leaders seeking to safeguard multifaceted health priorities amid ongoing and future public health emergencies.
Subject of Research:
Impact of the COVID-19 pandemic on mortality of hospitalized tuberculosis patients in Thailand, focusing on mediating roles of hospital caseload and severity.
Article Title:
Impact of COVID-19 pandemic, and the mediating role of hospital caseload and severity on mortality of hospitalised tuberculosis patients in Thailand.
Article References:
Zayar, N.N., Chotipanvithayakul, R., Geater, A.F. et al. Impact of COVID-19 pandemic, and the mediating role of hospital caseload and severity on mortality of hospitalised tuberculosis patients in Thailand. Glob Health Res Policy 10, 37 (2025). https://doi.org/10.1186/s41256-025-00437-7
Image Credits:
AI Generated