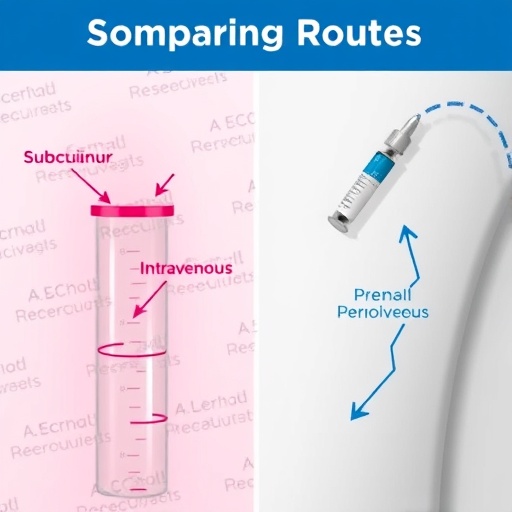
In the rapidly advancing field of oncology, the quest for optimized treatment regimens for metastatic non-small cell lung cancer (NSCLC) has led to innovative studies that delve into the efficacy and logistics of administering immunotherapies. A pivotal research piece recently published investigates the comparative analysis of subcutaneous versus intravenous administration of pembrolizumab, an immune checkpoint inhibitor, particularly when combined with chemotherapy. This study not only evaluates the therapeutic outcomes but also underscores the operational efficiencies of these two distinct delivery methods.
The focal point of this investigation lies in the burgeoning field of cancer immunotherapy, where pembrolizumab has emerged as a game changer in the treatment landscape for NSCLC. By targeting the programmed death receptor-1 (PD-1), pembrolizumab activates the immune system to more effectively recognize and attack cancer cells, marking a significant evolution from traditional chemotherapy approaches. Combining it with chemotherapy represents a strategic move to exploit synergies between therapies, potentially enhancing treatment efficacy, patient outcomes, and overall survival rates.
One of the most interesting aspects of this research is the methodology employed—the time and motion study framework. This analytical approach allows researchers to systematically evaluate the processes involved in the administration of both treatment modalities, quantifying the duration and resources needed to administer each version of pembrolizumab treatment. Such detailed insights are crucial for crafting more patient-friendly treatment protocols that can minimize time spent in clinical settings while maximizing therapeutic effectiveness.
As the authors delve deeper, they highlight the logistical challenges inherent in intravenous administration, including the need for vascular access and the potential for infusion-related reactions, which can lead to delays and increased resource consumption. In contrast, the subcutaneous route offers immediate benefits in terms of patient comfort and convenience, enabling a more streamlined administration process that could translate to reduced clinic visits. This aspect alone could revolutionize how healthcare facilities manage the increasing patient load seen in oncology departments.
Moreover, the study meticulously captures the patient experience, which is a vital component of treatment adherence and satisfaction. The psychological burden of frequent hospital visits and prolonged infusion times can detract from the overall treatment experience for patients battling cancer. By reducing the complexity and frequency of treatments through subcutaneous administration, there’s potential to significantly enhance quality of life, an essential consideration in long-term cancer management strategies.
An equally important theme emerging from the research is the cost-effectiveness of different administration methods. By evaluating administrative efficiencies through time spent with healthcare professionals and the associated resource allocation, the study offers valuable insights into a healthcare system under constant financial pressure. The findings may assist healthcare organizations in making informed decisions that align with value-based care principles, ultimately improving patient outcomes while managing costs effectively.
Clinical implications from this research extend beyond mere administration routes. Understanding the nuanced differences in pharmacokinetics, such as absorption rates and peak serum concentrations between the two modalities, opens doors for further research into individualized treatment plans. Tailoring therapies based on patient-specific characteristics—including their health status, cancer stage, and preferences—could herald a new era of personalized medicine in oncology.
The timing of this study is particularly relevant against the backdrop of a healthcare landscape still grappling with a global pandemic, where efficiency and patient safety are more critical than ever. With healthcare professionals and systems stretched thin, the ability to administer effective treatments with greater ease and efficiency can alleviate some of the burdens. The research thus serves as a timely reminder of the importance of innovation in clinical practice amid evolving global health challenges.
In conclusion, the comparative analysis of subcutaneous pembrolizumab versus its intravenous counterpart in conjunction with chemotherapy presents a compelling case for re-evaluating treatment protocols for metastatic NSCLC. The time and motion study brings to light the essential interplay between therapeutic efficacy, patient experience, and logistical practicality, paving the way for future advancements that prioritize both clinical outcomes and the holistic welfare of patients. As more studies emerge, it is these nuanced explorations that will ultimately shape the future direction of cancer care.
The integration of immunotherapy, specifically monoclonal antibodies like pembrolizumab, has changed the therapeutic landscape of lung cancer. However, the path ahead will require ongoing research and collaboration among professionals in oncology, healthcare delivery, and policy-making to ensure that advancements benefit patients comprehensively and sustainably in the years to come.
Ultimately, the findings from this pivotal study could represent not just a shift in how pembrolizumab is administered, but a broader change in the paradigm of cancer treatment—one that prioritizes efficiency, patient-centered care, and therapeutic outcomes, all critical in the fight against lung cancer and beyond.
Subject of Research: Comparative Analysis of Subcutaneous and Intravenous Pembrolizumab in NSCLC Treatment
Article Title: A Time and Motion Study Comparing Subcutaneous Pembrolizumab Versus Intravenous Pembrolizumab in Combination with Chemotherapy for the Treatment of Metastatic Non-small Cell Lung Cancer.
Article References:
De Cock, E., Oskar, S., Lourdudoss, C. et al. A Time and Motion Study Comparing Subcutaneous Pembrolizumab Versus Intravenous Pembrolizumab in Combination with Chemotherapy for the Treatment of Metastatic Non-small Cell Lung Cancer.
Adv Ther (2025). https://doi.org/10.1007/s12325-025-03365-7
Image Credits: AI Generated
DOI: 10.1007/s12325-025-03365-7
Keywords: Pembrolizumab, NSCLC, Immunotherapy, Time and Motion Study, Subcutaneous Administration, Intravenous Administration, Chemotherapy, Patient Experience, Oncology.