In a groundbreaking study set to make waves in the medical community, researchers from Japan have unveiled critical findings regarding the management of Type 1 Diabetes, specifically focusing on the risks associated with diabetic ketoacidosis (DKA) and severe hypoglycemia. The investigation compares the efficacy and safety of combining ipragliflozin, a sodium-glucose cotransporter 2 (SGLT2) inhibitor, with insulin versus insulin therapy alone. This real-world database study sheds light on the advantages and challenges of this novel treatment approach, showcasing a significant step in diabetes management.
Type 1 Diabetes, characterized by the autoimmune destruction of insulin-producing beta cells in the pancreas, presents unique challenges for patients and healthcare providers alike. Insulin therapy has traditionally been the cornerstone of treatment; however, recent advancements in pharmacotherapy, such as the introduction of SGLT2 inhibitors, have sparked interest in revising treatment paradigms. Ipragliflozin, one such agent, has shown promise in enhancing glycemic control and aiding weight management in Type 2 Diabetes patients, raising questions about its effectiveness in Type 1 Diabetes.
Amidst a backdrop of rising diabetes prevalence, the identification of potential risks associated with treatment options has become essential. Diabetic ketoacidosis, a life-threatening complication marked by hyperglycemia and ketone body accumulation, poses a serious risk for individuals with Type 1 Diabetes. On the other hand, severe hypoglycemia, characterized by critically low blood glucose levels, also remains a significant concern, often leading to severe neurological impairment or even death if untreated.
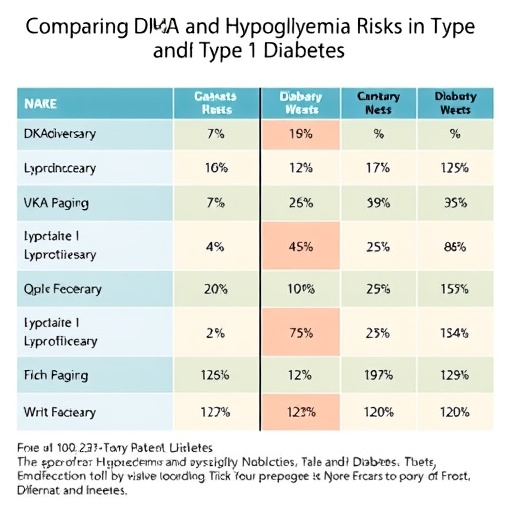
In this study, Kawamura et al. meticulously analyzed data from a vast Japanese database to explore the comparative risks of DKA and severe hypoglycemia in patients treated with a combination of ipragliflozin and insulin versus those receiving insulin therapy alone. By examining a carefully curated cohort, their investigation aimed to elucidate whether the addition of ipragliflozin could mitigate or exacerbate these risks.
The methodology employed in this research is noteworthy, as it reflects a robust approach to studying real-world scenarios rather than relying solely on controlled clinical trials, which often have stringent inclusion criteria. The authors employed statistical techniques to adjust for confounding factors, ensuring the validity of their findings. This aspect of the study underscores the importance of real-world evidence in understanding the complexities of diabetes management.
As the research progressed, the findings revealed a nuanced picture. While the combination therapy of ipragliflozin and insulin demonstrated potential benefits in terms of glycemic control, the data suggested a concerning uptick in DKA episodes among patients utilizing this treatment regimen. Conversely, incidents of severe hypoglycemia appeared to be lower in the combination therapy group, indicating a potential protective effect against this dangerous complication.
The implications of these findings extend far beyond the immediate context of the study. For clinicians, the insights derived from Kawamura et al.’s work may catalyze a re-evaluation of treatment strategies for Type 1 Diabetes. The dual-edged sword of improved glycemic control versus the heightened risk of DKA necessitates a careful balancing act in clinical practice, prompting further research into patient selection criteria and monitoring protocols.
Moreover, the study invites patients and healthcare providers alike to engage in informed discussions about treatment goals and preferences. The risks associated with DKA, particularly in combination therapy, highlight the necessity for comprehensive patient education. Patients must be aware of the symptoms of DKA and understand their individual risk profiles, empowering them to make informed decisions regarding their treatment options.
As researchers continue to uncover the multifaceted nature of diabetes management, the importance of patient-centered care becomes increasingly clear. It is essential for healthcare professionals to tailor treatment regimens to suit individual patient needs, taking into account their unique medical histories, lifestyle factors, and preferences. This approach not only enhances adherence but also fosters a collaborative dynamic between patients and providers.
Looking forward, the authors of this study call for further investigation into the long-term outcomes associated with the ipragliflozin and insulin combination therapy. The need for larger, multicenter trials is crucial in validating the findings of this Japanese study across diverse populations. As the medical community strives to optimize diabetes management, understanding the intricate relationship between treatment modalities and patient outcomes remains a top priority.
In conclusion, the research conducted by Kawamura and colleagues represents a significant contribution to the field of diabetes studies, shedding light on the implications of combining ipragliflozin with insulin therapy in Type 1 Diabetes management. The delicate balance between combating DKA risks while minimizing severe hypoglycemia events presents both challenges and opportunities, paving the way for a deeper understanding of how best to manage this complex disease. With continued research and application of these findings in clinical practice, there is hope that patients will receive more personalized, effective treatment regimens that enhance their quality of life while minimizing complications.
In an era where chronic diseases like diabetes exert a monumental toll on public health, it remains essential to prioritize research that elucidates new pathways for therapy. The collaborative efforts of researchers, clinicians, and patients will undoubtedly drive advancements, ultimately transforming the landscape of diabetes care for future generations.
Subject of Research: Risks of DKA and Severe Hypoglycemia in Type 1 Diabetes with Ipragliflozin/Insulin Therapy
Article Title: Diabetic Ketoacidosis and Severe Hypoglycemia Risks with Ipragliflozin/Insulin Versus Insulin in Type 1 Diabetes: A Japanese Real-World Database Study
Article References:
Kawamura, T., Lee, T., Shintani-Tachi, M. et al. Diabetic Ketoacidosis and Severe Hypoglycemia Risks with Ipragliflozin/Insulin Versus Insulin in Type 1 Diabetes: A Japanese Real-World Database Study.
Diabetes Ther (2025). https://doi.org/10.1007/s13300-025-01815-7
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s13300-025-01815-7
Keywords: Type 1 Diabetes, Diabetic Ketoacidosis, Severe Hypoglycemia, Ipragliflozin, Insulin, Real-World Database Study