Emerging from the shadows of geriatric research, frailty has gained recognition as a pivotal barometer for assessing older adults’ health. With the rising prevalence of frailty underscoring the need for refined measurement strategies, a groundbreaking study from Johnson et al. sheds light on the cumulative deficit model of frailty. This model represents an innovative leap forward in both survey and routine data methodologies. The relevance of this research cannot be overstated, as it holds the potential to transform how practitioners and researchers address the complexities of aging populations.
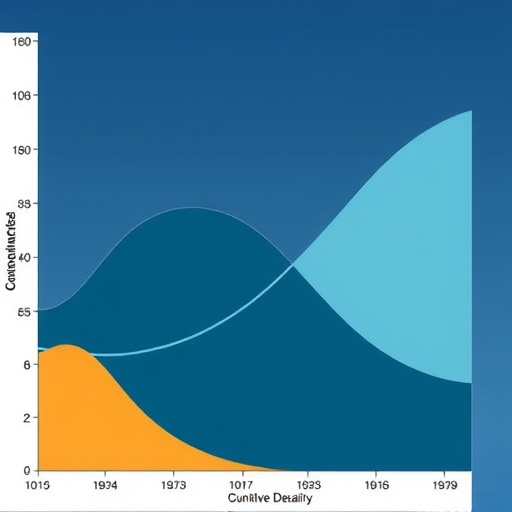
Traditionally, frailty has been a nebulous concept, encompassing aspects of diminished physiological reserve and increased vulnerability to stressors. The cumulative deficit model operationalizes this by quantifying health deficits—chronic conditions, disabilities, and other health-related variables that can cumulatively reflect an individual’s frailty status. What sets this study apart is its comparative analysis of how well this model performs across diverse data sources, including both survey-based inquiries and routine clinical data.
The researchers meticulously delineated their methodological approach, beginning with an extensive literature review. They aimed to establish a robust framework for assessing frailty, focused on the cumulative deficits presented in their model. The approach underscores the importance of not merely recognizing frailty but effectively measuring it in a way that yields actionable insights. Central to their analysis was the hypothesis that diverse data streams could yield converging insights about frailty, facilitating a more comprehensive understanding of health outcomes in older adults.
Utilizing longitudinal data added a rich layer of analysis to their research. By tracking health trajectories over time, the study presents a compelling narrative about how frailty evolves. The longitudinal aspect allows for a nuanced view of frailty, demonstrating that it is not a static condition but rather a dynamic process influenced by a myriad of factors. This perspective is crucial in geriatric medicine, where interventions often hinge on timely recognition and management of frailty.
Additionally, the researchers took deliberate steps to ensure that their methodology was both innovative and replicable. They engaged in rigorous statistical analyses designed to explore the nuances inherent in different datasets. This analytical depth highlights the complexity of frailty as a health outcome, inherently tied to individual health trajectories, making it essential to tailor assessments to reflect a person’s unique health status.
The implications of this research stretch far beyond academic discourse. With healthcare systems worldwide grappling with aging populations, the need for effective frailty assessment tools is more pronounced than ever. By refining the cumulative deficit model and validating its effectiveness across various data sources, Johnson and colleagues could well be paving the way for improved clinical practices. This paradigm shift could lead to enhanced screening protocols, ensuring that frail individuals receive the care and resources necessary to mitigate risks associated with their health status.
Moreover, the study advocates for a standardized approach to frailty assessment, which could foster consistency across healthcare settings. Such standardization is vital not only for individual patient care but also for broader public health strategies aimed at addressing the needs of aging populations. In particular, the cumulative deficit model could serve as a foundational framework guiding policy development and program implementation for elder care.
Collaborative efforts among clinicians, researchers, and policymakers are essential in translating the findings of this study into practice. By establishing partnerships that facilitate the integration of findings into existing healthcare frameworks, stakeholders can drive systemic improvements aimed at frailty prevention and management. This collaborative spirit is imperative in a field characterized by its complexity, where navigating the interplay of health conditions requires multifaceted strategies.
The findings of this study may also resonate in patient education programs. As the healthcare landscape evolves, empowering older adults with knowledge about frailty and its implications is vital. Understanding the risks associated with frailty and the potential for intervention could encourage proactive health management. Johnson et al.’s work contributes to a growing body of evidence advocating for informed patient engagement in healthcare decisions.
In conclusion, the research presented by Johnson et al. represents a significant step forward in our understanding of frailty, particularly through the lens of the cumulative deficit model. By offering comparative insights from both survey data and routine clinical records, the study enhances the discourse surrounding frailty assessment. As the older adult population continues to expand, the findings of this research underscore the urgency of developing effective measurement and intervention strategies.
Ultimately, the journey to improve frailty assessment is a collective responsibility that spans various sectors within society. Building awareness, fostering collaborations, and investing in research will be critical in shaping a future where the health of our aging populations is prioritized. The cumulative deficit model not only serves as an academic construct but as a beacon of hope for enhancing the quality of life for innumerable older adults navigating the complexities of frailty.
Subject of Research: Frailty assessment in older adults
Article Title: Measuring frailty: a comparison of the cumulative deficit model of frailty in survey and routine data
Article References:
Johnson, L., Guthrie, B., Anand, A. et al. Measuring frailty: a comparison of the cumulative deficit model of frailty in survey and routine data.
Eur Geriatr Med (2025). https://doi.org/10.1007/s41999-025-01251-7
Image Credits: AI Generated
DOI:
Keywords: frailty, cumulative deficit model, older adults, health assessment, geriatric care