In the rapidly advancing field of biomaterials, reliable cytotoxicity assessment remains a cornerstone for preclinical evaluations. A groundbreaking comparative study recently published in BioMedical Engineering OnLine for 2025 sheds new light on two widely employed cell viability assessment techniques—fluorescence microscopy (FM) and flow cytometry (FCM)—casting a spotlight on their performance when applied to particulate bioactive glasses. This study offers nuanced insights critical for researchers aiming to evaluate biomaterial biocompatibility with higher accuracy and precision.
Bioactive glass 45S5 (BG) has emerged as a promising candidate for bone-related applications due to its osteoconductive and biocompatible properties. However, its particulate nature introduces complex interactions with cells, making cytotoxicity evaluation nuanced and challenging. The study investigated SAOS-2 osteoblast-like cells exposed to BG particles spanning three distinct size ranges: less than 38 micrometers, between 63 and 125 micrometers, and 315 to 500 micrometers. These were tested under increasing concentrations of 25, 50, and 100 mg/mL over two exposure periods—three hours and seventy-two hours—capturing early and prolonged cellular responses.
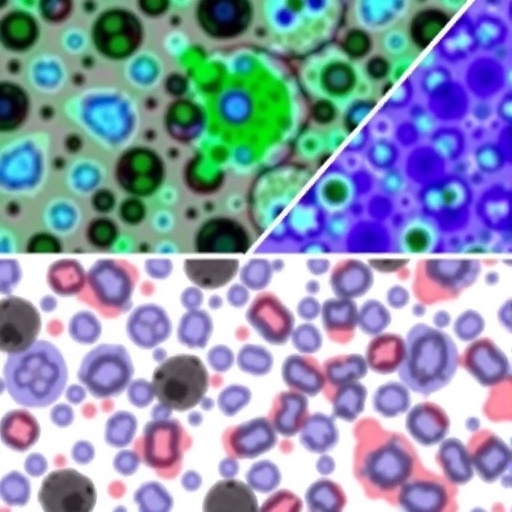
Fluorescence microscopy, utilizing FDA/PI staining protocols, served to differentiate viable from non-viable cells on a visual assessment basis. Meanwhile, flow cytometry pushed the boundaries of cell viability characterization by integrating multiparametric staining tools, including Hoechst dye, DiIC1, Annexin V-FITC, and PI. This enabled a more detailed categorization, not only into viable and nonviable populations but also distinguishing early versus late apoptotic states and necrosis. This multipronged staining approach permitted a subtler and more comprehensive understanding of cell fate under biomaterial exposure.
Both FM and FCM results revealed a compelling trend: smaller particle sizes and higher concentrations corresponded with heightened cytotoxic effects. Notably, exposure to particles smaller than 38 micrometers at the maximum concentration of 100 mg/mL profoundly reduced viability. Fluorescence microscopy reported a viability decrease to approximately 9% after 3 hours, which marginally increased to 10% after 72 hours. Contrastingly, flow cytometry registered even more dramatic results—viability plummeting to 0.2% at 3 hours and slightly recovering to 0.7% by 72 hours. This stark difference underscores the sensitivity and higher resolution of flow cytometry in detecting subtle cellular health variations.
Control groups maintained a robust viability exceeding 97%, reinforcing the conclusion that cytotoxicity was significantly dependent on particle size and dosage. Importantly, a strong statistical correlation between FM and FCM data was observed, with a correlation coefficient (r) of 0.94 and an R² value of 0.8879, alongside a p-value below 0.0001. This statistical agreement validates fluorescence microscopy as a viable screening tool, although it still lacks the precision offered by flow cytometry.
The real advantage of flow cytometry emerged in its ability to subdivide the apoptotic landscape. Whereas fluorescence microscopy generally dichotomizes cells into live or dead, FCM’s multiparametric approach allowed for the detection of early apoptotic changes prior to cell membrane breakdown, as well as differentiation of late apoptosis from outright necrosis. This nuanced capability is crucial in understanding cellular mechanisms triggered by particulate bioactive glass, offering a window into the processes of programmed cell death rather than mere end-point viability.
Furthermore, the superior precision of flow cytometry became most evident in conditions of elevated cytotoxic stress. When bioactive glass concentration and particle size hit the thresholds inducing marked toxicity, FCM could reliably detect subtle variations that fluorescence microscopy could not discern. This makes FCM invaluable for studies where accurate quantification under extreme stress conditions is essential, potentially influencing both biomaterial design and safety assessments.
This pioneering work not only establishes the size- and dose-dependent cytotoxic potential of Bioglass 45S5 but also elevates the status of flow cytometry as an advanced, quantitative technique for cytocompatibility evaluation. Researchers working in particulate biomaterials now have compelling evidence to adopt flow cytometry for detailed viability assessments, enabling refined interpretations that could accelerate biomaterial optimization for clinical applications.
Considering the importance of biomaterials in regenerative medicine and implants, this study is poised to influence the standards for preclinical cytotoxicity testing. The ability to discriminate apoptotic stages and necrotic death with high accuracy facilitates more informed decisions regarding biomaterial safety and efficacy. It also underscores the need to consider particle size distribution more critically, as smaller particles pose disproportionately higher risks.
The implications transcend technical methodology, extending to translational research and regulatory frameworks. Flow cytometry’s enhanced precision ensures that potential cytotoxic effects are not underestimated, fortifying the safeguards before clinical translation. This could mitigate unforeseen cytotoxic side effects, improving patient safety and treatment outcomes.
Moreover, the methodological rigor displayed in this investigation sets a benchmark for future studies examining cytotoxicity in complex particulate systems. By integrating complementary staining paradigms and performing time-course assessments, the approach provides a comprehensive picture of cellular health dynamics influenced by biomaterials.
In a landscape dominated by the urgent need for biocompatible materials, this research decisively steers the community towards more sensitive, multi-parameter viability assessments. Flow cytometry’s ability to reveal the apoptotic trajectory offers new strategies for early detection of cytotoxic responses, enhancing predictive modeling of biomaterial compatibility and facilitating safer biomaterial innovation.
Looking ahead, the fusion of advanced flow cytometry techniques with emerging high-throughput platforms promises to further revolutionize cytotoxicity evaluations. This could pave the way for rapid, multiplexed analyses across numerous biomaterial candidates, accelerating the development pipeline.
In summary, this seminal study highlights the transformative potential of flow cytometry over conventional fluorescence microscopy in evaluating cell viability following exposure to particulate bioactive glass. The findings emphasize that particle size and concentration critically modulate cytotoxicity and that a detailed multiparametric approach affords a superior understanding of cellular responses. As biomaterial research moves towards increasingly sophisticated platforms, the insights from this work will undeniably shape experimental protocols and safety evaluations across biomedical engineering disciplines.
Subject of Research: Cytotoxicity assessment of particulate bioactive glass (Bioglass 45S5) on osteoblast-like cells using fluorescence microscopy and flow cytometry.
Article Title: Evaluating cell viability assessment techniques: a comparative study of flow cytometry and fluorescence microscopy in response to bioactive glass exposure.
Article References:
Samuel, B.J., Jin, Z., Brauer, D.S. et al. Evaluating cell viability assessment techniques: a comparative study of flow cytometry and fluorescence microscopy in response to bioactive glass exposure. BioMed Eng OnLine 24, 112 (2025). https://doi.org/10.1186/s12938-025-01452-y
Image Credits: AI Generated