In an unprecedented dive into the genomic landscape of a significant pathogen, researchers led by Tewolde have embarked on a comprehensive comparative genomic analysis of Mycoplasma pneumoniae, the bacterium responsible for a range of respiratory infections, in the United Kingdom over an eight-year span from 2016 to 2024. This seminal work, recently published in the journal BMC Genomics, sheds light on the genetic variations and evolutionary dynamics of this elusive microbe, which poses a constant threat to public health. The findings pave the way for enhanced diagnostics, treatment strategies, and surveillance protocols required to tackle Mycoplasma pneumoniae infections.
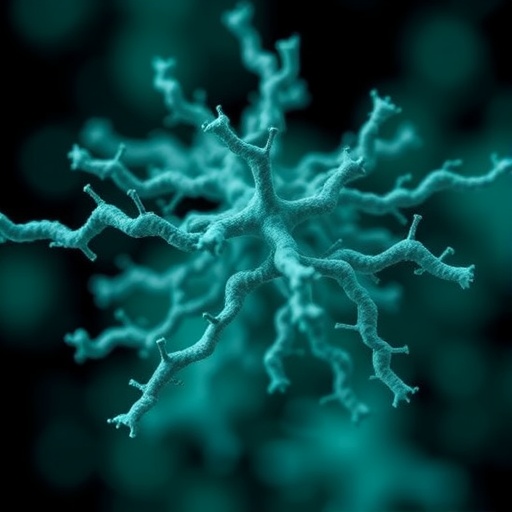
Mycoplasma pneumoniae has garnered considerable attention in the scientific community due to its unique morphological features and its status as a leading cause of atypical pneumonia worldwide. Lacking a cell wall, this bacterium is notoriously difficult to culture and study in laboratory settings, making genomic analysis a critical tool for understanding its pathogenicity and resistance mechanisms. Over the years, advancements in sequencing technologies have empowered researchers to decode the genomic makeup of various strains, offering unprecedented insights into their evolutionary trajectories.
The backdrop for this study is especially crucial, given the changing environmental conditions and the impact of healthcare practices over recent years. With the rise of antibiotic-resistant strains, the need to analyze the genomic data of Mycoplasma pneumoniae from different geographical regions and timeframes has become more pressing than ever. Tewolde’s team meticulously gathered isolates from various clinical sources, ensuring a representative sample that reflects the contemporary genetic diversity of Mycoplasma pneumoniae in the United Kingdom.
Employing state-of-the-art sequencing techniques, the researchers generated extensive genomic data that illuminated key mutations and structural variations across the strains. The application of comparative genomics allowed for a nuanced understanding of how these variations correlate with clinical manifestations of the infections caused by Mycoplasma pneumoniae. By analyzing canonical genes associated with virulence and antibiotic resistance, the team could elucidate the genetic underpinnings that contribute to the bacterium’s adaptability in human hosts.
One notable outcome of the genomic analysis was the identification of specific genetic markers linked to antibiotic resistance. The emergence of resistant strains has been a growing concern in medicine, and this study provides critical data that can inform future treatment protocols. For instance, the research highlighted particular mutations in genes associated with macrolide resistance, marking a pivotal step in understanding how Mycoplasma pneumoniae evades the effects of commonly prescribed antibiotics, thus posing significant challenges for clinicians.
In addition to examining resistance mechanisms, the genomic study also revealed information about the evolutionary pressures exerted on Mycoplasma pneumoniae populations over the examined period. By comparing historical sequences with more recent isolates, the researchers tracked how various strains have evolved in response to changes in treatment regimens and public health interventions. This retrospective look is invaluable for predicting future trends in bacterial evolution and pathogenicity, further underscoring the relevance of genomic studies in contemporary microbiology.
Beyond its clinical ramifications, the study of Mycoplasma pneumoniae also plays a vital role in our understanding of bacterial ecology. The findings from Tewolde et al. add to a growing body of literature advocating for the integration of genomic analysis into routine surveillance of respiratory pathogens. The ability to rapidly identify and characterize strains can significantly enhance outbreak responses, enabling healthcare protocols to adapt swiftly to the emergence of new variants.
As the implications of this work unfold, it is essential to consider the broader context of respiratory infections. With the COVID-19 pandemic underscoring the importance of respiratory health on a global scale, the study’s timing is particularly pertinent. Researchers can draw parallels between the lessons learned from Mycoplasma pneumoniae and other viral and bacterial pathogens, fostering a more integrated approach to respiratory illness management and prevention strategies.
The potential for interdisciplinary collaboration is vast. The genomic insights collected by Tewolde and collaborators could inspire further research into associated respiratory conditions, leading to improved diagnostic tests and therapeutic options. As we move deeper into the genomic era of medicine, the dialogue between microbiologists, clinicians, and epidemiologists becomes increasingly crucial.
Overall, this groundbreaking research not only highlights the importance of continuous genomic surveillance but also calls for a re-evaluation of how Mycoplasma pneumoniae is approached in clinical settings. The emergence of new strains and the continuous adaptation of existing populations underscore the necessity for integrated health responses that are agile and informed by genomic data.
In conclusion, Tewolde et al.’s analysis illustrates the transformative power of genomics in understanding complex pathogens like Mycoplasma pneumoniae. As the scientific community absorbs and builds upon these findings, there is hope that this work will catalyze advancements in diagnosing and managing respiratory infections, ultimately contributing to improved health outcomes on a global scale.
Understanding the interplay between bacterial genetics and clinical outcomes remains paramount as we navigate the complexities of infectious diseases in a post-pandemic world. The contributions made by this research lay a critical foundation for future studies aimed at combating respiratory pathogens effectively. By continually harnessing and applying genomic technologies, we can not only track the path of pathogens but also anticipate their future trajectories in an ever-changing health landscape.
Subject of Research: Comparative genomic analysis of Mycoplasma pneumoniae.
Article Title: Comparative genomic analysis of Mycoplasma pneumoniae isolated in the United Kingdom, between 2016 and 2024.
Article References:
Tewolde, R., D’Aeth, J.C., Thombre, R. et al. Comparative genomic analysis of Mycoplasma pneumoniae isolated in the United Kingdom, between 2016 and 2024.
BMC Genomics 26, 893 (2025). https://doi.org/10.1186/s12864-025-12101-y
Image Credits: AI Generated
DOI:
Keywords: Mycoplasma pneumoniae, comparative genomics, antibiotic resistance, respiratory infections, genomic surveillance.