Recent advances in medical imaging are transforming the way we understand cerebrovascular health, particularly in pediatric populations. A groundbreaking study conducted by researchers Smith, Lewis, and Zhang explores the use of unsedated cerebrovascular reactivity imaging (uCVI) in children. This innovative technique not only sheds light on the dynamics of cerebral blood flow but also emphasizes the importance of performing such analyses without the use of sedation. Sedation can complicate the assessment of pediatric patients and poses inherent risks, making the findings of this research particularly significant.
Cerebrovascular reactivity refers to the ability of cerebral blood vessels to change their diameter in response to various stimuli, which can indicate the health of the brain’s vascular system. Traditional modalities of assessing this reactivity in children often required sedation, which could alter physiological responses and necessitate additional medical oversight. The authors aimed to develop a technique that would allow this critical evaluation while maintaining the child’s natural state, providing more reliable data about their cerebrovascular health.
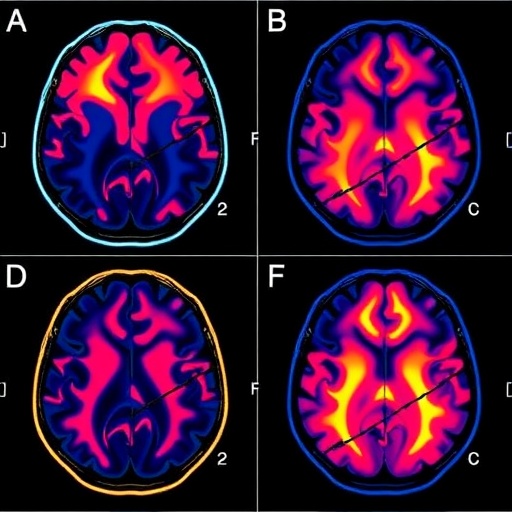
In this study, enlisted children underwent uCVI during their routine medical evaluations. Utilizing near-infrared spectroscopy (NIRS) as a primary imaging tool, the researchers measured changes in blood flow in response to specific stimuli, such as breath-holding. This particular approach allows for non-invasive and real-time monitoring of cerebral hemodynamics. The results were promising: children displayed a high tolerance for the procedure, which suggests that the method could potentially be adopted more widely in clinical practice.
Additionally, the study highlighted how the absence of sedation reduced the risk factors for adverse events commonly associated with sedation in pediatric patients. Unsedated procedures lessen the burden on families and healthcare providers alike, avoiding the potential complications of anesthesia. This new technique not only addresses clinical needs but also aligns with trends toward patient-centered care in pediatric healthcare.
The findings detailed in this research present a vital opportunity for healthcare professionals to assess cerebrovascular function more transparently and efficiently. As pediatric neurologists and radiologists explore the implications of these results, they may be compelled to reconsider established protocols regarding cerebral blood flow monitoring in young patients.
Moreover, this study advocates for further exploration into unsedated imaging techniques across other domains of pediatric diagnostic imaging. The importance of developing child-friendly medical technologies is underscored, aiming to facilitate positive experiences during potentially stressful evaluations. By reducing the need for sedation, this technique can alleviate anxiety not just for the child undergoing the scan, but also for their families.
The implications of this research extend far beyond the realm of pediatric imaging. Understanding cerebrovascular reactivity is crucial for identifying various neurological disorders that can affect children, including migraines, cerebrovascular accidents, and other neurodevelopmental challenges. This knowledge is essential for tailoring prevention strategies and interventions to enhance children’s overall neurological health.
The study’s authors emphasize the potential of uCVI in comparing healthy children to those with neurological conditions, providing insight into differences in cerebrovascular reactivity that could aid in diagnosis and treatment planning. This approach could lead to earlier intervention strategies, positively impacting outcomes for children facing various neurological challenges.
Furthermore, the findings align with growing research into the relationship between cerebrovascular health and cognitive function in children. Enhanced understanding of how cerebral blood flow responds to different stimuli could illuminate connectivity between vascular health and cognitive development, ultimately informing educational strategies and support systems for affected children.
This considerable shift in the paradigm of cerebrovascular assessment in pediatric medicine could influence future research and medical practices. The alignment of technology, children’s best interests, and safety underscores the commitment of modern medicine to advancing techniques that prioritize health and well-being.
As this research gains attention, it is imperative for medical institutions and practices to consider integrating uCVI into their imaging protocols for pediatric patients. Training and infrastructure may need to evolve to accommodate the growing popularization of this innovative method. Given the profound implications of cerebrovascular health on child development, such an evolution in practice could have far-reaching consequences.
In conclusion, unsedated cerebrovascular reactivity imaging represents a significant advancement in pediatric neurology. The pioneering work by Smith and colleagues lays the groundwork for further exploration into unsedated imaging techniques, with the ultimate goal of improving the safety and efficacy of neurological evaluations in children. As the field expands, equitable access to such innovative procedures will be crucial in transforming pediatric healthcare and ensuring the best possible outcomes for future generations.
The commitment to harnessing new technologies while prioritizing the needs of pediatric patients embodies the future of medical imaging. With the potential to refine diagnostic accuracy and bolster clinical understanding, the promise of unsedated cerebrovascular assessments illuminates new pathways in child health and medical research.
Subject of Research: Unsedated cerebrovascular reactivity imaging in children.
Article Title: Unsedated cerebrovascular reactivity imaging is well-tolerated in children.
Article References:
Smith, A.E., Lewis, J.B., Zhang, J. et al. Unsedated cerebrovascular reactivity imaging is well-tolerated in children.
Pediatr Radiol (2025). https://doi.org/10.1007/s00247-025-06350-y
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s00247-025-06350-y
Keywords: Pediatric imaging, cerebrovascular reactivity, unsedated techniques, near-infrared spectroscopy, neurological health.