A groundbreaking study published in the latest issue of npj Parkinson’s Disease unveils a transformative approach to predicting levodopa-induced dyskinesia (LID) in Parkinsonian models through advanced cerebral perfusion imaging. This pioneering research introduces a new frontier in understanding the neural dynamics that precede the debilitating motor complications associated with chronic levodopa therapy, illuminating pathways that could radically alter both prognostic assessments and therapeutic strategies for Parkinson’s disease (PD).
Levodopa, the gold standard in symptomatic treatment of Parkinson’s disease, is often shadowed by the emergence of dyskinesias—erratic, involuntary movements that significantly compromise quality of life. Despite extensive efforts, clinicians have been persistently challenged by the unpredictable onset and severity of LID, which emerges in a subset of patients undergoing long-term levodopa regimens. Therefore, a predictive biomarker capable of forecasting LID prior to its clinical manifestation holds immense promise for individualized treatment optimization and the mitigation of side effects.
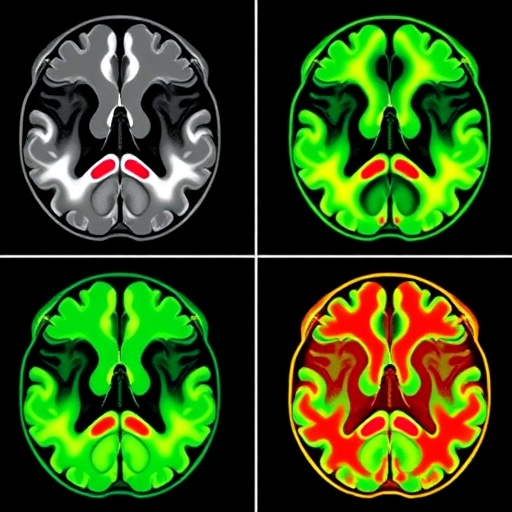
In this innovative study, the authors employed cerebral perfusion imaging techniques to monitor and quantify regional blood flow changes within key motor and non-motor brain regions in a well-established Parkinsonian rat model. The experimental design meticulously replicated the progressive dopaminergic neurodegeneration characteristic of PD and chronic levodopa administration to simulate the bio-behavioral environment conducive to dyskinesia development. Through longitudinal imaging and behavioral assessments, a consistent correlation between altered perfusion patterns and emerging dyskinetic phenotypes was demonstrated.
The cerebral perfusion metrics revealed that hyperperfusion in discrete subcortical structures, notably the putamen and globus pallidus, preceded the overt manifestation of dyskinesia by several days. This temporal dissociation suggests that vascular dynamics within the basal ganglia complex could serve as an early, noninvasive biomarker for LID risk stratification. Moreover, the imaging allowed for the spatial resolution of perfusion anomalies, offering unprecedented insight into network-specific pathophysiology rather than global brain changes. These findings challenge the traditional neurochemical-centric paradigm and underscore the importance of vascular contributions in dyskinetic pathogenesis.
Crucially, the study detailed the longitudinal evolution of cerebral perfusion changes during the course of levodopa treatment. Initial hypoperfusion associated with dopaminergic neuronal loss was observed, followed by a compensatory hyperperfusion phase correlating with dyskinesia onset. Such biphasic vascular responses delineate a dynamic cerebrovascular adaptation that may underlie maladaptive synaptic plasticity and excitotoxicity responsible for motor fluctuations. By establishing this perfusion trajectory, the research opens doors for temporal intervention points to modify disease progression.
In addition to regional perfusion abnormalities, the researchers explored perfusion heterogeneity, quantifying blood flow variability within the motor circuitry. Heightened heterogeneity was found to parallel the complexity and severity of dyskinetic movements, implying that not only absolute perfusion values but also their spatial distribution dynamics influence symptomatic expression. This nuanced understanding offers a potential metric to track disease state and therapeutic efficacy beyond conventional clinical scoring systems.
Methodologically, the study leveraged cutting-edge arterial spin labeling (ASL) magnetic resonance imaging (MRI), a noninvasive technique sensitive to cerebral blood flow that eliminates the need for exogenous contrast agents. This advantages allow longitudinal measurements without interfering with physiological processes, critical for chronic experimental paradigms. The use of ASL-MRI in small animal models presents technical challenges due to spatial resolution constraints and motion artifacts, which the team adeptly overcame through custom hardware adaptations and sophisticated image processing algorithms.
From a translational standpoint, the findings herald exciting prospects for developing perfusion-based diagnostic tools applicable in clinical settings. Early detection of LID vulnerability could facilitate tailored dosing regimens, implementation of adjunctive therapies, or consideration of alternative pharmacologic agents to avert dyskinesia. Furthermore, cerebral perfusion imaging might complement existing biomarkers—genetic, biochemical, and electrophysiological—to enrich predictive models and enhance personalized Parkinson’s care.
The study also highlighted potential mechanistic insights connecting cerebral blood flow alterations with neuroinflammatory processes and blood-brain barrier integrity disruptions that accompany levodopa therapy. Perfusion changes may reflect underlying microvascular remodeling or endothelial dysfunction contributing to pathological neural circuit hyperactivity. Such intersections between vascular biology and neurodegeneration are rapidly gaining recognition, prompting a reevaluation of therapeutic targets that encompass cerebrovascular health alongside neurotransmitter restoration.
Notably, the rat model’s recapitulation of human LID phenotypes strengthens the ecological validity of the results, underscoring the relevance of perfusion imaging to human disease. Nevertheless, the authors acknowledge that interspecies differences necessitate cautious extrapolation and advocate for future clinical trials employing advanced perfusion MRI in PD patients under levodopa treatment to validate these preclinical findings.
In the broader context of movement disorder research, this study exemplifies the power of multimodal neuroimaging to decode the complex interplay of vascular and neuronal factors driving disease manifestations. It challenges researchers to adopt holistic frameworks encompassing neurovascular coupling, synaptic plasticity, and metabolic shifts to unravel the intricate biology of Parkinson’s disease and its treatment complications.
The potential clinical impact is profound: personalized therapeutic interventions informed by cerebral perfusion patterns could minimize LID incidence, prolong levodopa efficacy, and improve patient quality of life. Moreover, integrating perfusion imaging into routine neurological assessments might redefine prognostic criteria and stimulate the innovation of neuroprotective strategies targeting cerebrovascular mechanisms.
In conclusion, this landmark study delineates cerebral perfusion imaging as a transformative predictive tool for levodopa-induced dyskinesia, bridging fundamental neuroscience with practical clinical application. Its findings invite a paradigm shift emphasizing vascular contributions to PD therapeutic outcomes and underscore the critical need for interdisciplinary research leveraging neuroimaging, pharmacology, and vascular biology to combat this debilitating disorder.
As Parkinson’s disease continues to impose a growing public health burden globally, insights emerging from sophisticated imaging modalities promise not only to enhance scientific understanding but to directly benefit patients by refining diagnosis, guiding therapy, and ultimately alleviating one of the most challenging complications of long-term levodopa administration.
Subject of Research:
Cerebral perfusion imaging as a predictive biomarker for levodopa-induced dyskinesia in a Parkinsonian rat model.
Article Title:
“Cerebral perfusion imaging predicts levodopa-induced dyskinesia in Parkinsonian rat model.”
Article References:
Perron, J., Krak, S., Booth, S. et al. Cerebral perfusion imaging predicts levodopa-induced dyskinesia in Parkinsonian rat model. npj Parkinsons Dis. 11, 278 (2025). https://doi.org/10.1038/s41531-025-01133-6
Image Credits: AI Generated