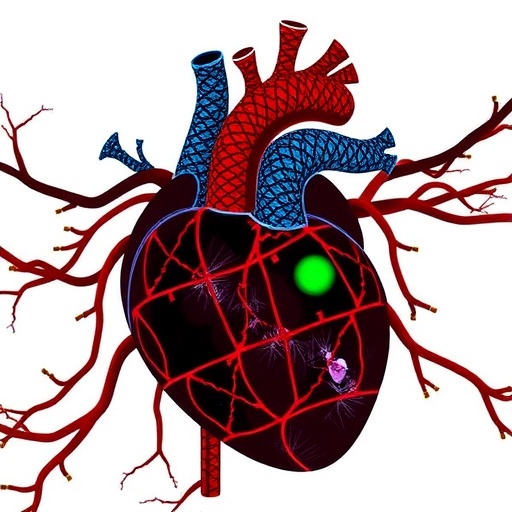
In a groundbreaking discovery that could reshape the future of regenerative cardiology, researchers have unveiled a critical molecular pathway that significantly enhances the heart’s ability to heal following a myocardial infarction. The study, recently published in Nature Communications, elucidates the role of the chemokine CCL28 in stimulating angiogenesis and facilitating cardiac repair after heart attacks, specifically through its action on CCR10-positive endothelial cells in male mice. This revelation opens the door to potential new therapies aimed at improving heart recovery and function after ischemic injury.
Myocardial infarction, commonly known as a heart attack, remains one of the leading causes of morbidity and mortality globally. Following the ischemic event, the heart tissue suffers extensive damage due to the lack of blood supply, and the innate repair mechanisms of the heart are often insufficient to fully restore its function. A critical aspect of cardiac repair involves revascularization—the formation of new blood vessels in the damaged myocardium, a process known as angiogenesis. However, the molecular drivers modulating this process in the context of heart injury have remained only partially understood, limiting the development of targeted therapies.
The study conducted by Yang, Chen, Lyu, and colleagues identifies CCL28, a chemokine traditionally associated with immune cell trafficking and mucosal immunity, as a pivotal regulator of angiogenesis in the post-infarct heart. Their sophisticated in vivo experiments demonstrate that CCL28 expression is significantly upregulated in the cardiac tissue of male mice soon after myocardial infarction, correlating with enhanced neovascularization and improved cardiac function. This expanded understanding that CCL28 extends beyond immune modulation to influence endothelial biology marks a paradigm shift.
Endothelial cells, which line the inner surface of blood vessels, play an essential role in angiogenesis. The authors found that a subpopulation of these cells expressing the receptor CCR10 is the primary target through which CCL28 exerts its pro-angiogenic effects. By binding to CCR10, CCL28 activates intracellular signaling pathways that promote the proliferation, migration, and tube formation capabilities of endothelial cells, all critical steps in new vessel formation. This precise cell-type specificity adds an important layer to our knowledge of how targeted molecular interactions can orchestrate complex tissue repair processes.
Utilizing advanced genetic models, the research team was able to show that knocking out either CCL28 or its receptor CCR10 leads to a marked reduction in post-infarction angiogenesis and worsened cardiac function, highlighting the indispensable role of this signaling axis. Conversely, therapeutic administration of recombinant CCL28 or strategies to augment CCR10 expression on endothelial cells enhanced vascular regeneration and significantly attenuated myocardial damage. These findings robustly suggest the pathway as a promising therapeutic target to boost endogenous cardiac repair mechanisms after infarction.
The implications of these discoveries are profound, considering the limited regenerative capacity of the adult mammalian heart and the current lack of effective treatments that can restore lost myocardium. By focusing on the CCL28-CCR10 axis, future therapies might be able to harness or mimic this natural regenerative signal, offering hope for patients who suffer from chronic heart failure secondary to ischemic injury. Such interventions could improve survival rates and quality of life by preserving ventricular function and preventing adverse remodeling.
Moreover, the study sheds light on the sexual dimorphism of cardiac repair mechanisms, with the authors specifying their findings in male mice. This points to a need for further investigation to unravel whether similar pathways operate in females and how sex hormones might modulate the response. Understanding these nuances is crucial given the well-recognized differences in cardiovascular disease presentation and outcomes between men and women, and could guide more personalized therapeutic approaches.
The research also contributes to a broader framework of cardiac biology by linking chemokine signaling to vascular regeneration, a concept that may extend to other ischemic conditions beyond the heart. By identifying CCR10-expressing endothelial cells as key effectors, the results provide a cellular target for bioengineering and regenerative medicine strategies, including cell-based therapies and biomaterials designed to deliver angiogenic signals locally.
In addition, the mechanistic insights offered by this study emphasize the importance of the stromal microenvironment in cardiac repair. CCL28 secreted by damaged myocardial tissue not only recruits immune cells but also directly activates endothelial cells, illustrating a dual function in orchestrating the repair milieu. This complex interplay between immune signaling and vascular biology is a frontier area of research that could reveal multifaceted intervention points.
The rigorous experimental design involved in vivo lineage tracing, gene knockout models, and functional assays, coupled with state-of-the-art imaging techniques to quantify neovascularization, strengthens the validity and translational relevance of the findings. The study sets a benchmark for future research into chemokines’ non-immune functions in tissue regeneration.
However, while the murine model provides compelling evidence, transferring these findings into clinical practice will require overcoming significant challenges. These include verifying the relevance of CCL28-CCR10 signaling in human heart disease, optimizing delivery mechanisms for therapeutic modulation, and ensuring safety given the delicate balance of chemokine networks in inflammation and repair.
Nonetheless, the identification of CCL28 as an angiogenic factor represents a landmark discovery that could inspire a wave of innovative treatments addressing the unmet needs in cardiovascular medicine. Coupled with advances in gene therapy, nanotechnology, and biomaterials, targeting the CCL28-CCR10 pathway may soon transition from bench to bedside.
This pioneering work also encourages a reassessment of chemokines in other degenerative diseases where vascular dysfunction is prominent. The broad applicability of chemokine modulation highlights the interdisciplinary potential of this research in regenerative medicine.
Furthermore, the study invites a deeper exploration of the temporal dynamics of chemokine expression following injury, emphasizing that timing may be crucial in maximizing therapeutic efficacy. It underscores the necessity of precision medicine approaches in the orchestration of tissue repair.
In conclusion, the work by Yang and colleagues not only expands our molecular understanding of post-infarction cardiac repair but also provides a compelling therapeutic avenue that combines immunology and vascular biology. As the population ages and cardiovascular disease remains a dominant global health challenge, such innovative strategies herald a new era in cardiac regenerative therapies with the potential to save millions of lives worldwide.
Subject of Research: The role of the chemokine CCL28 and CCR10+ endothelial cells in promoting angiogenesis and cardiac repair after myocardial infarction in male mice.
Article Title: CCL28 contributes to angiogenesis and cardiac repair through CCR10+ endothelial cells after myocardial infarction in male mice.
Article References:
Yang, K., Chen, H., Lyu, Y. et al. CCL28 contributes to angiogenesis and cardiac repair through CCR10+ endothelial cells after myocardial infarction in male mice. Nat Commun 16, 9262 (2025). https://doi.org/10.1038/s41467-025-64283-4
Image Credits: AI Generated