In a groundbreaking study published in BMC Pediatrics, researchers have uncovered critical insights into the role of CCL2, a pro-inflammatory factor, in liver diseases, particularly in biliary atresia. This condition, which primarily affects infants and results in the obstruction of bile flow, leads to severe liver damage and inflammation. The work conducted by Li, Liu, Li, and colleagues emphasizes how CCL2 enhances the interactions between monocyte-macrophage cells and liver parenchymal cells, which are pivotal in the progression of liver inflammation and subsequent fibrosis. Such findings open new avenues for understanding the pathophysiological mechanisms that underlie biliary atresia and could potentially guide future therapeutic strategies.
The researchers initiated their investigation by characterizing the cellular interactions involved in biliary atresia. The liver contains various cell types, including hepatocytes, cholangiocytes, and immune cells such as monocytes and macrophages. Under normal conditions, these cells communicate and maintain homeostasis. However, in biliary atresia, the balance is disrupted, leading to inflammation and fibrotic changes. This complex interplay is vital for understanding how inflammatory responses in the liver can contribute to the chronic progression of the disease.
One of the standout findings of this study was the identification of CCL2 as a significant player in mediating the crosstalk between monocyte-macrophage cells and liver parenchymal cells. CCL2, also known as monocyte chemoattractant protein-1 (MCP-1), is a chemokine that attracts monocytes to sites of inflammation. Its elevated levels have been associated with various liver diseases, but its specific role in biliary atresia had not been fully elucidated until this research.
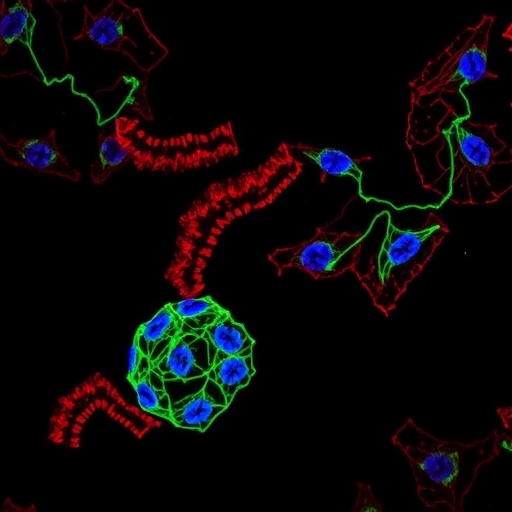
The authors employed advanced techniques such as flow cytometry and immunofluorescence microscopy to assess the interactions between these cell types. They discovered that CCL2 not only attracted monocytes to the inflamed liver but also altered the behavior of macrophages once they arrived. These recruited macrophages exhibited a pro-inflammatory phenotype, thereby perpetuating the inflammatory cycle and exacerbating tissue damage. This revelation highlights the importance of CCL2 in driving the inflammatory processes that characterize biliary atresia.
In addition to demonstrating CCL2’s role in inflammation, the study also explored its effects on liver fibrosis. Fibrosis in the liver is characterized by the excessive accumulation of extracellular matrix components, leading to scarring and impaired liver function. The researchers showed that the interaction between macrophages and liver parenchymal cells, mediated by CCL2, significantly contributes to the fibrogenic processes in biliary atresia. This discovery brings new understanding into how inflammation drives fibrosis and underlines the potential of targeting CCL2 as a therapeutic strategy.
The study also highlighted gender differences in the inflammatory and fibrotic responses, a factor that complicates our understanding of biliary atresia. Notably, the authors found variations in CCL2 expression levels between male and female subjects, suggesting that sex hormones may influence the severity of liver inflammation and fibrosis. This insight is crucial because it indicates that potential therapies targeting CCL2 could be more effective when tailored to individual patient profiles, considering such biological differences.
Building on the findings of this research, future studies will undoubtedly aim to explore potential therapeutic interventions. If CCL2 is indeed a driving force behind the inflammation and fibrosis in biliary atresia, then inhibiting its activity may ameliorate disease progression. Researchers are now investigating the efficacy of CCL2 inhibitors in preclinical models, which could lead to innovative treatment modalities for this debilitating condition.
Furthermore, the implications of this study extend beyond biliary atresia. Chronic liver inflammation is a common denominator in numerous liver diseases, ranging from alcoholic liver disease to non-alcoholic fatty liver disease and even hepatocellular carcinoma. The insights gained from understanding CCL2’s role could pave the way for targeted therapies not only for biliary atresia but also for a spectrum of liver pathologies that share similar inflammatory mechanisms.
The study’s innovative findings and methodological rigor provide a robust framework for future research. By further dissecting the signaling pathways involved in CCL2-mediated interactions, scientists could uncover new molecular targets for intervention. Additionally, the exploration of biomarkers associated with CCL2 may enhance early diagnosis and prognostic evaluation, ultimately improving patient outcomes.
In conclusion, the work of Li and colleagues presents compelling evidence that CCL2 plays a critical role in the pathology of biliary atresia by facilitating interactions between macrophages and liver parenchymal cells, leading to exacerbated inflammation and fibrosis. The potential of CCL2 as a therapeutic target represents a significant leap forward in the pursuit of effective treatments for biliary atresia and other liver diseases characterized by chronic inflammation. The ramifications of this research are deep and wide-ranging, offering hope for improving therapeutic strategies that could transform the clinical management of these conditions.
Understanding the full implications of this study will require ongoing research, but the current findings serve as a beacon for neurobiology and pediatric gastroenterology. With further elucidation of the mechanisms at play, researchers are poised to develop interventions that may mitigate the severe consequences of biliary atresia and restore liver health in affected infants.
As new data emerge, this research underscores the necessity for integrated and multidisciplinary approaches in tackling pediatric liver diseases. By bridging laboratory findings with clinical applications, the scientific community can move closer to resolving the challenges posed by such complex conditions.
Subject of Research: Role of CCL2 in liver inflammation and fibrosis in biliary atresia.
Article Title: Inflammatory factor CCL2 enhances the interaction between monocyte-macrophage cells and liver parenchymal cells to promote liver inflammation and fibrosis in biliary atresia.
Article References: Li, X., Liu, S., Li, T. et al. Inflammatory factor CCL2 enhances the interaction between monocyte-macrophage cells and liver parenchymal cells to promote liver inflammation and fibrosis in biliary atresia. BMC Pediatr 25, 643 (2025). https://doi.org/10.1186/s12887-025-05984-z
Image Credits: AI Generated
DOI:
Keywords: CCL2, biliary atresia, liver inflammation, fibrosis, pediatric liver disease, macrophages, chemokines.