A Revolutionary Leap in Cancer Therapy: The Promise and Challenges of In Vivo CAR T Cell Production
Chimeric Antigen Receptor T cell (CAR T) therapy has emerged as a transformative modality in oncology, particularly for hematological malignancies that have resisted traditional treatment modalities. Despite its remarkable clinical successes, the production pipeline of CAR T cells remains a bottleneck, characterized by labor-intensive steps, prolonged timelines, and exorbitant costs that impede widescale application. The advent of in vivo CAR T cell production presents a groundbreaking shift in therapeutic strategy, promising to disrupt the conventional paradigm by streamlining manufacturing and enhancing accessibility.
Conventional CAR T cell therapy requires a multi-step ex vivo process involving the isolation of a patient’s T cells, their activation, genetic modification, expansion, and rigorous quality control assays. This workflow commonly extends over two to three weeks, during which time delicate cellular manipulations can compromise T cell functionality, and rapid disease progression may outpace treatment availability. Furthermore, the personalized nature of such therapies restricts scalability, confining benefits to select patients within specialized centers.
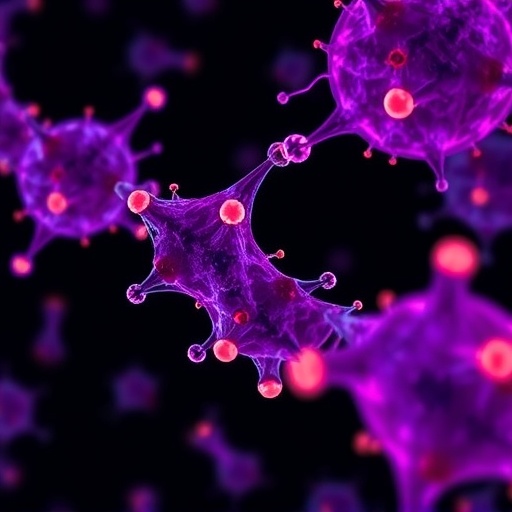
The cutting edge concept of in vivo CAR T cell production foregoes extracorporeal cell processing by delivering CAR genetic constructs directly into T cells within the patient’s body. This approach utilizes finely engineered viral vectors, such as lentiviruses and adeno-associated viruses (AAVs), alongside emerging nonviral delivery systems, including lipid nanoparticles. Upon administration, these vectors specifically transduce T cells in situ, effectuating genetic reprogramming that endows them with tumor-targeting capabilities. This innovation has the potential to drastically reduce production complexities, cut timelines, and improve therapeutic potency by preserving T cell phenotypes in their native milieu.
One of the foremost advantages of in vivo CAR T therapy lies in its inherent scalability and potential to yield “off-the-shelf” CAR T cell products. Contrasting with the “one patient, one batch” model of ex vivo manufacturing, in vivo strategies could harness a more universal delivery modality, enabling broader patient reach and cost efficiencies unimaginable with current standards. Moreover, retaining T cells within their physiological environment mitigates the risk of functional exhaustion seen in cultured cells, thus enhancing efficacy and durability of tumor eradication.
Nanoparticle-based delivery systems exemplify a promising nonviral vector class facilitating efficient CAR gene transfection with minimal immunogenicity. Their ability to encapsulate nucleic acids and traverse biological barriers allows for targeted T cell modification without integrating viral components, thereby alleviating concerns regarding insertional mutagenesis. Advances in materials science have led to the design of nanoparticles optimized for stability, biodistribution, and cell-specific uptake, which are critical parameters for clinical translation.
Viral vectors such as lentiviruses and AAVs remain pivotal due to their high transduction efficiency and ability to confer stable CAR expression. Lentiviral vectors integrate into the T cell genome, ensuring persistent CAR expression, whereas AAVs tend to remain episomal, offering a safer but transient modification profile. The refinement of vector tropism and promoter elements continues to improve transgene expression specificity and intensity, enhancing the precision of in vivo CAR T cell engineering.
Despite the promise, the transition to in vivo CAR T cell production is not without formidable challenges. Precise targeting is essential to avoid off-target modification of non-T cell populations, which could provoke adverse effects or diminish therapeutic efficacy. Immunogenic responses to vector components or newly expressed CAR proteins pose risks of rapid clearance, reduced transgene expression, or systemic inflammation. Additionally, insertional mutagenesis induced by integrating vectors remains a safety concern necessitating rigorous preclinical assessment.
The rapidly progressing biology of certain malignancies makes the expedited timeline of in vivo CAR T cell generation especially compelling. Bypassing ex vivo expansion could dramatically shorten the interval between diagnosis and treatment administration, potentially altering disease trajectories. Furthermore, overcoming manufacturing bottlenecks could democratize access to CAR T therapy beyond specialized centers, fostering more equitable cancer care.
An important consideration in advancing in vivo CAR T therapies is balancing transfection efficiency with cost-effectiveness and safety profiles. While viral vectors offer superior gene transfer efficiencies, their production costs and biosafety infrastructure requirements can be prohibitive. Conversely, nonviral systems promise more affordable manufacturing and flexibility but often suffer from lower transduction rates. Intensive research aims to optimize these platforms, perhaps combining the strengths of both approaches to achieve the ideal therapeutic index.
Ongoing studies are exploring the integration of synthetic biology and genome editing tools to refine the specificity and functionality of in vivo-generated CAR T cells. Innovations such as inducible CAR expression systems and multispecific CAR constructs may be harnessed to enhance tumor targeting while minimizing off-tumor toxicity. Additionally, multiplexed delivery systems could facilitate simultaneous modification of multiple immune cell types, broadening the scope of adoptive immunotherapy.
In summary, in vivo CAR T cell therapy stands at the frontier of personalized medicine, poised to overcome the scalability and logistical obstacles of traditional CAR T manufacturing. Its capacity for rapid, efficient, and cost-effective generation of functional CAR T cells could revolutionize clinical oncology, especially for aggressive cancers needing urgent intervention. While challenges surrounding safety, targeting specificity, and delivery vector optimization remain, the trajectory of current research augurs well for the translation of this approach into routine clinical practice.
The evolution of CAR T cell engineering from complex ex vivo bioprocesses to streamlined in vivo genetic modification mirrors the broader trend in gene therapy toward minimally invasive, patient-centric interventions. As the field progresses, collaborative efforts among immunologists, bioengineers, and clinicians will be paramount to harnessing the full potential of in vivo CAR T cell production, ultimately transforming the landscape of cancer treatment and patient outcomes.
Subject of Research: In vivo production of CAR T cells and its therapeutic potential in cancer treatment.
Article Title: In vivo production of CAR T cell: Opportunities and challenges.
News Publication Date: 1-Nov-2025.
References: Zhiqiang Song, Yi Zhou, Binbin Wang, Yuke Geng, Gusheng Tang, Yang Wang, Jianmin Yang, In vivo production of CAR T cell: Opportunities and challenges, Genes & Diseases, Volume 12, Issue 6, 2025, 101612, DOI: 10.1016/j.gendis.2025.101612.
Image Credits: Genes & Diseases.
Keywords: Cancer genetics, CAR T cell therapy, in vivo CAR T production, gene therapy, viral vectors, nanoparticle delivery, hematological malignancies, immunotherapy.