In a groundbreaking study conducted by researchers at Harbin Medical University, the intricate landscape of the tumor microenvironment in acute promyelocytic leukemia (APL) patients undergoing arsenic trioxide (ATO) therapy has been meticulously unveiled through advanced single-cell sequencing techniques. This pioneering work delineates the heterogeneity within APL cell populations, providing unprecedented insight into the cellular dynamics underpinning therapeutic responses.
The investigation commenced by categorizing APL cells into distinct and functionally diverse subpopulations. Among these, a particularly elusive leukemic stem cell (LSC)-like subset was discerned, characterized by elevated expression levels of stemness-associated genes and a robust LSC transcriptional signature. This subpopulation is implicated as the pivotal driver of differentiation arrest that defines APL pathology. Crucially, ATO treatment was shown to markedly deplete this LSC-like compartment, elucidating a potential mechanism by which ATO induces remission.
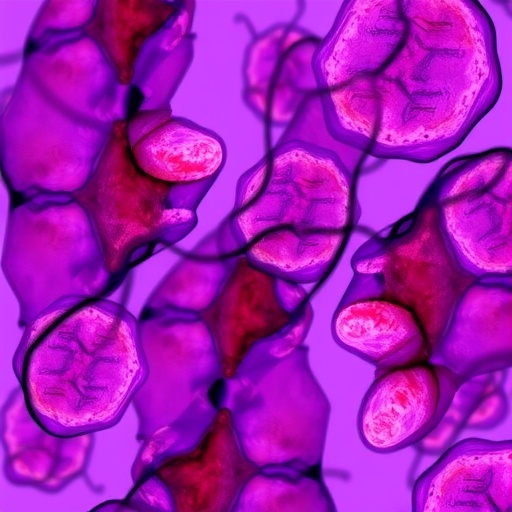
Immune system components, especially lymphocytes such as T cells, natural killer (NK) cells, and B cells, represent fundamental players in antitumor immune surveillance and response. Delving deeper, the researchers identified that ATO therapy precipitates a significant enrichment of a CD8+ T cell subset characterized by the upregulation of interferon-stimulated genes (ISGs), hence termed the CD8 ISG subtype. This population not only displayed heightened effector functions post-treatment but also exhibited notable expansion in T cell receptor (TCR) clonotypes, underscoring its potential immunologic vigor in the therapeutic milieu.
A comprehensive co-expression network analysis further unveiled that the CD8 ISG subtype holds a multifaceted transcriptional program. Beyond the ISG signature, this subset demonstrated gene expression profiles linked to myeloid differentiation pathways, arsenic response elements, and broader immune activation signatures, suggesting its integral role at the nexus of immunological and leukemic cell interplay following arsenic exposure.
Parallel investigations into NK cell compartments revealed a contrasting functional dichotomy. Pre-treatment NK cells in APL patients were found to be functionally impaired, exhibiting phenotypes consistent with immune exhaustion or dysfunction. Remarkably, ATO therapy restored NK cell functionality, giving rise to an activated NK subset marked by pronounced nuclear factor kappa B (NFκB) signaling and robust inflammatory activation, signaling a reinvigoration of innate immune responses triggered by ATO.
The integration of single-cell RNA sequencing (scRNA-seq) with single-cell B cell receptor sequencing (scBCR-seq) brought to light dynamic remodeling of immunoglobulin repertoires following ATO administration. These alterations reflect a profound reshaping of humoral immunity, potentially contributing to sustained antileukemic effects and improved immune surveillance post-treatment.
Dissecting the complex cellular communication networks within the bone marrow niche, the study identified the lymphotoxin (LT) signaling pathway as a critical mediator facilitating cross-talk between the newly characterized CD8 ISG and NK NFκB subpopulations and APL blasts. This interaction axis appears central to orchestrating myeloid differentiation and modulating immune activation, positioning the LT pathway as a promising therapeutic target to enhance ATO efficacy.
This comprehensive single-cell omics analysis not only deciphers the cellular and molecular reprogramming induced by ATO in the APL tumor microenvironment but also spotlights novel immunological subpopulations pivotal for therapeutic success. The identification of CD8 ISG T cells and NK NFκB cells as key players in the antileukemic immune response heralds new avenues for immunomodulatory strategies complementing existing regimens.
Furthermore, the study highlights the transformative potential of single-cell multi-omics approaches in oncology, offering unparalleled resolution to decode tumor-immune dynamics and treatment resistance mechanisms. The detailed transcriptional landscapes established pave the way for biomarker discovery and rational design of combination therapies aimed at eradicating residual disease and preventing relapse.
The profound immune remodeling observed suggests that ATO does more than target malignant cells directly; it effectively reconditions the host immune ecosystem to mount a potent and coordinated antitumor response. This dual modality underscores the therapeutic promise of integrating targeted cytotoxic agents with immune-stimulating interventions.
By delineating the molecular underpinnings of ATO’s impact on both leukemic cells and the immune microenvironment, this work provides compelling evidence for revisiting current treatment paradigms in APL and potentially other hematological malignancies. The findings advocate for patient monitoring strategies that incorporate immune profiling to optimize individualized therapy and predict clinical outcomes.
In sum, this investigation not only expands fundamental understanding of APL pathobiology under arsenic trioxide therapy but also establishes a robust platform for future translational research. The potential to manipulate identified immune subsets and signaling pathways holds promise for enhancing remission durability and improving patient prognoses in this aggressive leukemia subtype.
This landmark research was supported by multiple prestigious funding bodies including the National Key Research and Development Program of China, the National Natural Science Foundation of China, and the Heilongjiang Province Natural Science Foundation. Collaborative efforts and advanced computational analyses underpinned the successful execution of this multi-dimensional study, setting a new standard in leukemia research.
Subject of Research: Tumor microenvironment remodeling in acute promyelocytic leukemia under arsenic trioxide therapy
Article Title: Single-cell omics analysis reveals tumor microenvironment rewiring after arsenic trioxide therapy in acute promyelocytic leukemia
Web References: http://dx.doi.org/10.1016/j.scib.2025.09.014
Image Credits: ©Science China Press
Keywords: Acute promyelocytic leukemia, arsenic trioxide therapy, single-cell sequencing, tumor microenvironment, leukemic stem cells, CD8 T cells, interferon-stimulated genes, natural killer cells, NFκB signaling, immune activation, lymphotoxin pathway, hematopoietic lineage rewiring