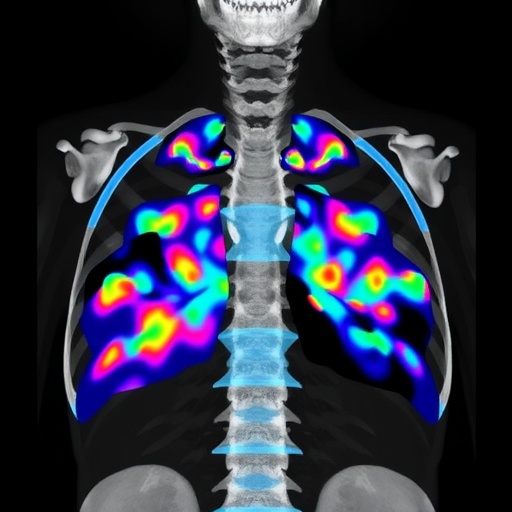
Differentiated thyroid cancer (DTC) is commonly associated with a relatively favorable prognosis, but the emergence of bone metastases (BM) adds a challenging layer of complexity to patient outcomes. Recent advances in imaging techniques, specifically radioactive iodine (RAI) scans and fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography (^18F-FDG PET/CT), have unveiled distinct patterns of uptake in bone lesions that appear to harbor critical prognostic significance. A groundbreaking study published in BMC Cancer now delves deeply into how these uptake patterns influence clinical outcomes and survival rates in patients with metastatic DTC.
Bone metastases in thyroid cancer patients represent an advanced disease state often refractory to conventional treatments. This study scrutinizes the diagnostic and prognostic potential of combining RAI and ^18F-FDG PET/CT uptake patterns from 67 patients treated over a 15-year period. The researchers meticulously classified the patients into three categories based on their bone lesion uptake: those with RAI-positive but PET-negative lesions (RAI+/PET-), those positive on both RAI and PET scans (RAI+/PET+), and those negative on RAI but positive on PET imaging (RAI-/PET+). This stratification forms the backbone of the study’s novel insights.
Intriguingly, the study uncovered that the RAI+/PET+ group dominated the cohort, representing nearly 60% of the patients, while the RAI+/PET- and RAI-/PET+ groups comprised smaller proportions. These uptake patterns correlated profoundly with clinical outcomes, suggesting a biological basis for the metabolic behavior observed through imaging. This nuanced approach challenges previous one-dimensional interpretations of metastatic thyroid cancer progression.
One of the study’s central findings highlights the RAI(+) ratio—the proportion of bone lesions exhibiting RAI uptake—as a powerful determinant of progression-free survival (PFS) and overall survival (OS) within the RAI+/PET+ subgroup. Patients with more than 50% of lesions demonstrating RAI positivity exhibited significantly improved clinical trajectories, with extended median PFS and OS periods compared to those with lower ratios. This suggests that the extent of iodine avidity in bone metastases retains a prognostic gravity even amidst FDG-avidity, a marker traditionally associated with aggressive disease.
Moreover, a pivotal advance in this research comes from the employment of total lesion glycolysis (tTLG), a quantitative PET/CT imaging biomarker that integrates both tumor volume and metabolic activity. tTLG emerged as an independent prognostic factor in multivariate analyses for both PFS and OS, underscoring its valuable role in risk stratification and therapeutic decision-making. The capacity to measure tTLG could revolutionize tailoring patient-specific management strategies in metastatic DTC, optimizing treatment efficacy and surveillance intensity.
Underlying these observations is the suggestion that RAI+/PET+ patients exhibit biological behaviors akin to RAI+/PET- patients rather than RAI-/PET+ cases. This parallels the hypothesis that the dual uptake pattern signifies a phenotype retaining differentiation features amenable to RAI therapy, contrasting with the more dedifferentiated and metabolically active PET-only positive lesions. The identification of this subclassification holds potential to refine risk assessment and personalize targeted interventions.
Histopathological and biochemical variables, including serum thyroglobulin levels and patient age, were also corroborated as significant covariates affecting survival outcomes. These findings resonate with existing literature emphasizing the multifactorial nature of prognosis in advanced thyroid cancer and fortify the need for comprehensive multimodal assessment integrating imaging, laboratory, and clinical parameters.
Notably, the study spans data accrued over 15 years, reflecting a robust longitudinal perspective on therapeutic outcomes in a rare and complex patient subset. All subjects underwent standardized ^131I treatment protocols, allowing for a uniform appraisal of RAI responsiveness in relation to imaging phenotypes. The rigorous methodological design and extended follow-up enhance the credibility and clinical applicability of these insights.
This research underlines the integral value of combining anatomical, functional, and metabolic imaging modalities in illuminating the pathobiology of bone metastatic DTC. Such multiparametric imaging approaches could refine the clinician’s ability to forecast disease trajectory, facilitating early intervention adjustments that may prolong survival and maintain quality of life.
For the medical community, these findings signal the dawn of more precise prognostic tools leveraging uptake patterns beyond conventional staging criteria. This could pave the way for stratifying patients who may benefit from intensified RAI therapy or adjunctive treatments targeting high metabolic activity lesions identified through ^18F-FDG PET/CT.
Furthermore, the study stimulates vital discourse regarding the biological underpinnings dictating differential tracer uptake in metastatic lesions, hinting at evolving tumor heterogeneity during disease progression. Future research elucidating molecular correlates of these imaging phenotypes may unlock novel therapeutic targets aimed at overcoming treatment resistance.
In conclusion, the integration of RAI and ^18F-FDG PET/CT uptake patterns, particularly the quantification of the RAI(+) ratio and tTLG, emerges as a transformative paradigm in prognostic evaluation for DTC patients with bone metastases. The implications for personalized medicine are profound, urging oncologists and nuclear medicine specialists to adopt this dual-imaging strategy to optimize patient outcomes in this challenging clinical scenario.
As advances continue, this study’s insights into the prognostic independence of tTLG and the clinical relevance of RAI uptake ratios herald a promising era of precision oncology in thyroid cancer. The synthesis of imaging biomarkers with clinical parameters will likely redefine therapeutic algorithms, tailoring interventions to the metabolic profile and iodine avidity of metastatic lesions.
Such strides underscore the indispensable role of nuclear imaging innovations in cancer management, enabling more than mere detection but offering deep prognostic and therapeutic guidance. Patients harboring metastatic DTC deserve this precision, which has the potential to inform risk-adapted therapies and ultimately improve longevity and quality of life.
This landmark research not only enriches the scientific comprehension of thyroid cancer metastasis but also charts a clear clinical pathway for enhancing prognostic accuracy and treatment personalization through integrative imaging biomarkers. The convergence of metabolic imaging and clinical oncology thus represents a frontier of hope and improved therapeutic stewardship.
Subject of Research: Clinical outcomes influenced by bone metastasis uptake patterns in differentiated thyroid cancer
Article Title: Clinical outcomes by bone metastasis uptake pattern in differentiated thyroid cancer
Article References:
Wang, G., Feng, F., Huang, S. et al. Clinical outcomes by bone metastasis uptake pattern in differentiated thyroid cancer. BMC Cancer 25, 1617 (2025). https://doi.org/10.1186/s12885-025-15036-5
Image Credits: Scienmag.com