In the frontier of neonatal health, the struggle against necrotizing enterocolitis (NEC) continues to challenge clinicians and researchers alike. NEC remains one of the most devastating gastrointestinal emergencies affecting premature infants, characterized by inflammation and bacterial invasion of the intestinal wall, leading to tissue necrosis. Despite advances in neonatal care, morbidity and mortality rates remain alarmingly high, underscoring an urgent need for innovative prevention and treatment strategies.
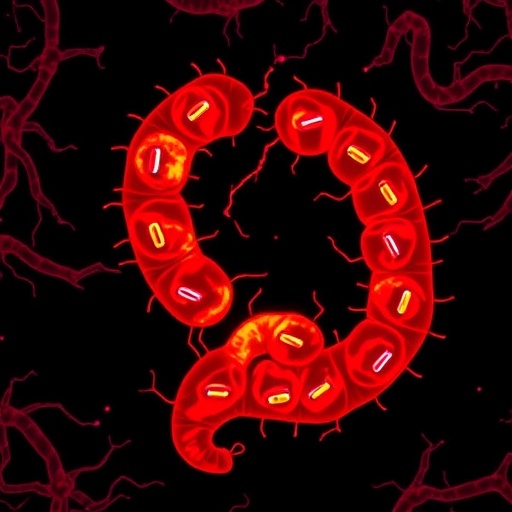
Recent groundbreaking research has now unveiled a fascinating biological mechanism that may revolutionize our understanding and management of NEC. At the heart of this discovery lies Limosilactobacillus reuteri, a gut commensal bacterium well-regarded for its probiotic properties. Yet, the novelty comes with the identification of its biofilm state, a structural bacterial community mode that crucially modulates host cellular pathways to confer protection against NEC.
Biofilms, long described in microbiology for their complexity and resilience, are structured communities of bacteria embedded within an extracellular matrix. This state facilitates enhanced bacterial survival and interaction with host tissues but has often been implicated in pathogenic contexts. This study throws new light on biofilm formation by beneficial bacteria, revealing that the biofilm state of L. reuteri exerts a protective effect through modulation of the aryl hydrocarbon receptor (AhR).
AhR is a cytosolic transcription factor with a broad influence on immune regulation, cellular differentiation, and mucosal integrity. It functions as a sensor for various endogenous and exogenous ligands, coordinating a sophisticated immunological response. By demonstrating that the biofilm state of L. reuteri upregulates AhR activity, the researchers have linked microbial community behavior directly to host immune modulation in the gut. This connection could be the mechanistic key that dampens the dysregulated inflammatory response characteristic of NEC.
Experimental models of NEC have traditionally employed rodent systems subjected to hypoxia and formula feeding to mimic preterm infant conditions. Using such models, the investigators administered biofilm-phase L. reuteri and monitored disease outcomes alongside molecular signaling pathways. Remarkably, the animals receiving this biofilm form of the probiotic exhibited significantly reduced intestinal injury, inflammation, and mortality rates compared to controls.
Delving deeper than phenotypic observations, the study elucidated how biofilm-associated metabolites from L. reuteri interact with AhR ligands within the intestinal microenvironment. This interaction appears to promote intestinal barrier function by enhancing tight junction protein expression, reducing epithelial permeability—a critical factor in preventing bacterial translocation that precipitates NEC pathology.
This elegant mechanistic insight also strengthens the concept of the microbiome as a dynamic immunoregulatory entity rather than a mere collection of commensal organisms. The capacity of L. reuteri biofilms to induce AhR reflects an evolved symbiosis where bacterial community structures fine-tune host responses to maintain homeostasis and prevent hyperinflammation.
Furthermore, the study underscores a fundamental temporal aspect—the state of the bacterium matters. Traditional probiotic administration often focuses on planktonic, free-living cells; however, this research advocates for leveraging biofilm-derived probiotics, a paradigm shift that may enhance therapeutic efficacy and durability within the neonatal gut.
The translational implications are profound. Current clinical probiotic protocols for NEC prevention could potentially be optimized by selecting strains capable of robust biofilm formation or by developing delivery systems that promote biofilm establishment in the infant gut. This biofilm-mediated modulation of AhR may serve as a biomarker or therapeutic target for individualized NEC prophylaxis.
Moreover, these findings resonate beyond neonatal care. Because AhR signaling pathways intersect with broader gastrointestinal diseases characterized by inflammation and epithelial barrier dysfunction, such as inflammatory bowel disease, this research opens vistas for probiotic applications across diverse clinical conditions.
The integration of microbial biofilm biology with host immune receptor signaling exemplifies the interdisciplinary rigor propelling modern microbiome science. This study’s use of comprehensive in vivo models, combined with molecular and biochemical assays, paints a cohesive picture of symbiotic interaction at cellular and community levels.
Equally exciting is the prospect of engineering probiotics with enhanced biofilm-forming capacities or synthetic biology approaches to harness and amplify beneficial host-microbe dialogues. The future may witness tailored probiotic therapies that act not only through microbial colonization but via orchestrated modulation of host receptor networks.
While promising, challenges remain before clinical translation. Ensuring consistency of biofilm formation in the variable and immature gastrointestinal milieu of preterm infants must be addressed. Additionally, safety and dosing parameters require rigorous evaluation to avert unintended consequences of manipulating immune pathways in delicate neonatal populations.
The study also invites reexamination of microbial ecology principles within the developing gut. Understanding how early-life factors such as antibiotic exposure, feeding practices, and environmental influences affect biofilm dynamics could further optimize microbiota-targeted interventions in neonatal care.
In sum, this research marks a paradigm-defining advancement linking the biofilm lifestyle of a key probiotic species to the modulation of host receptor activity and suppression of devastating intestinal disease. As we unravel the language of microbial communities speaking through molecular receptors, a new era in precision microbiome therapeutics dawns.
By harnessing the nuanced interplay between L. reuteri biofilms and AhR signaling, neonatal medicine moves closer to unlocking nature’s intrinsic solutions for NEC—a condition that has long evaded definitive prevention. Continued exploration at this intersection promises to illuminate not only NEC pathogenesis but broader immune-microbial symbioses vital for lifelong health.
The future is increasingly clear: the biofilm mode of life for beneficial bacteria holds untapped therapeutic potential. Through rigorous science and innovative clinical application, these insights herald a novel frontier in safeguarding the most vulnerable patients—our infants—ushering in hope for healthier beginnings worldwide.
Subject of Research:
Interaction between biofilm-forming Limosilactobacillus reuteri, aryl hydrocarbon receptor activity, and experimental necrotizing enterocolitis suppression.
Article Title:
Biofilm state Limosilactobacillus reuteri modulates aryl hydrocarbon receptor activity and suppresses experimental necrotizing enterocolitis
Article References:
Sajankila, N., Dumbauld, Z., Wang, Y. et al. Biofilm state Limosilactobacillus reuteri modulates aryl hydrocarbon receptor activity and suppresses experimental necrotizing enterocolitis. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04351-z
Image Credits:
AI Generated