Revolutionizing Skin Health: Unlocking ATG9A’s Role in Preventing Inflammatory Skin Disorders
The skin serves as the body’s primary defense against environmental onslaughts, acting not merely as a physical shield but also as an active immune organ. Recent groundbreaking research from VIB and Ghent University has unveiled a crucial molecular mechanism that safeguards the skin from debilitating inflammatory diseases, potentially opening transformative therapeutic pathways for conditions like psoriasis and lupus. This comprehensive study, published in Immunity on October 20, 2025, shines a spotlight on ATG9A, a protein governing autophagy, a cell’s intracellular waste management system, pivotal for immune regulation in the skin.
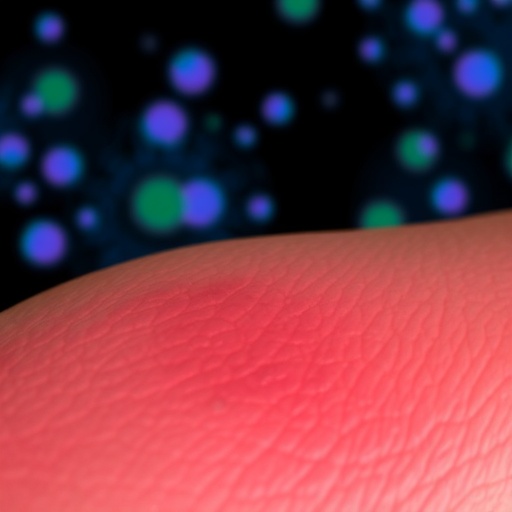
Controlled cell death, a process scientifically termed apoptosis, is essential for maintaining healthy skin turnover. Typically, when skin cells undergo apoptosis, the immune system efficiently clears these dying cells, maintaining homeostasis. However, aberrations arise when excessive cell death occurs either en masse or via pathological routes, serving as a distress signal that precipitates chronic inflammatory skin conditions. Researchers keenly investigated how intracellular cleanup mechanisms, specifically autophagy mediated by ATG9A, thwart such detrimental immune alarms to preserve skin integrity.
Autophagy is the cellular process of degrading and recycling damaged organelles and proteins—a fundamental maintenance pathway ensuring cell survival under stress. ATG9A acts as a critical regulator facilitating the delivery of cellular waste to lysosomes for degradation. Employing sophisticated genetically engineered mouse models alongside human patient sample analysis, the research team demonstrated that loss of ATG9A in keratinocytes—the predominant skin cells—provokes pronounced inflammatory skin diseases. This phenotype is characterized by a dramatic escalation in skin cell death and a disruption of the skin’s protective barrier, prompting an uncontrollable inflammatory cascade.
Detailed mechanistic insights revealed that ATG9A exercises its protective role by preventing the accumulation of pro-inflammatory proteins within the cytoplasm of skin cells. In the absence of ATG9A, these harmful proteins aggregate, triggering multiple inflammatory signaling pathways. Intriguingly, ATG9A orchestrates a non-canonical autophagy pathway—distinct from classical routes—that remains largely uncharted but is evidently indispensable for downregulating inflammatory mediators within the skin’s microenvironment.
At the molecular crossroads of this complex regulation lies the interplay between tumor necrosis factor (TNF) and type I interferons (IFNs), two cytokines instrumental in mediating skin inflammation. Traditionally, TNF and IFNs were considered independent contributors to pathological inflammation. This study, however, uncovers a tightly intertwined axis wherein TNF precipitates an aberrant IFN response. This pathological signaling relay is amplified through the activation of ZBP1, a sentinel protein known for detecting damaged nucleic acids, which further exacerbates keratinocyte death and tissue damage when unchecked by ATG9A.
The revelation that the TNF–IFN–ZBP1 signaling axis operates synergistically to fuel inflammatory skin diseases is paradigm-shifting. It challenges past therapeutic strategies that targeted individual cytokines, such as anti-TNF agents commonly prescribed for psoriasis. Although effective, these biologics often trigger significant adverse effects, including heightened infection risk and immune dysregulation. By pinpointing ATG9A’s central role in curbing this axis, the study identifies a promising molecular target that could lead to more precise, safer therapeutic modalities, potentially overcoming the limitations of current treatments.
Furthermore, the implications of this discovery transcend dermatology, as similar dysregulated inflammatory mechanisms involving excessive IFN responses are hallmarks of systemic inflammatory disorders including rheumatoid arthritis and inflammatory bowel disease. Targeting the ATG9A-regulated pathway could therefore pioneer innovative interventions across a spectrum of chronic inflammatory diseases, offering hope for millions of patients worldwide.
“The ability of ATG9A to direct inflammatory proteins toward autophagic degradation highlights an elegant cellular strategy to containing immune responses within skin cells,” stated Dr. Dario Priem, first author of the study. “It functions as a master suppressor, simultaneously modulating numerous inflammatory pathways and preserving skin homeostasis.” His insights emphasize the sophistication of intracellular quality control systems in immune regulation and their potential exploitation for therapeutic gain.
The research team’s utilization of advanced murine models deficient in ATG9A within the epidermis provided compelling causal evidence for the protein’s indispensable role. Mice lacking ATG9A recapitulated key features of human inflammatory skin disease, including epidermal thickening, keratinocyte apoptosis, and elevated pro-inflammatory cytokine production. Complementary patient data corroborated these findings, revealing diminished ATG9A expression levels in affected skin tissues, underscoring the clinical relevance.
Underlying this protective mechanism is the enigmatic STING pathway—a cytoplasmic sensor of DNA damage and stress that promotes inflammatory gene expression via type I interferon induction. The study revealed that ATG9A deficiency exacerbates STING activation downstream of TNF receptor 1 (TNFR1), integrating autophagic disruption with interferon-mediated inflammation. This discovery hints at a complex molecular nexus that couples cellular housekeeping to the modulation of innate immune sensors in skin biology.
From a translational perspective, the study advocates for the development of novel pharmacological agents aimed at enhancing ATG9A function or mimicking its autophagic activity. Such interventions might suppress the pathogenic TNFR1-STING-ZBP1 inflammatory cascade without broadly suppressing the immune system, preserving defensive immunity while preventing pathological damage. This approach stands to revolutionize treatment paradigms not only in dermatology but also in autoimmune and inflammatory medicine.
Prof. Mathieu JM Bertrand, senior author and immunologist at VIB-UGent, remarked, “Our elucidation of ATG9A’s role provides a fresh vista on immune regulation within the skin. Targeting this pathway could enable clinicians to intercept inflammatory diseases at their molecular roots with unparalleled precision. This research propels us closer to tailored, next-generation therapies that address unmet clinical needs in chronic inflammation.”
In conclusion, the identification of ATG9A-mediated autophagy as a pivotal mechanism underpinning the containment of skin inflammation represents a major leap forward in understanding the interface between cellular homeostasis and immune modulation. By unraveling the crosstalk between TNF and interferon signaling and its regulation through a specialized autophagy pathway, these findings lay the groundwork for innovative treatments that could dramatically improve the quality of life for individuals afflicted with inflammatory skin disorders and beyond.
Subject of Research: Animals
Article Title: ATG9A-mediated autophagy prevents inflammatory skin disease by limiting TNFR1-driven STING activation and ZBP1-dependent cell death.
News Publication Date: 20 October 2025
Keywords: Diseases and disorders, Health care, Health and medicine, Cell biology, Immunology, Life sciences