AT1R Autoantibodies and Fetal Hepatic Glycogen Synthesis: A Groundbreaking Discover
In a groundbreaking study published by Bian et al., researchers delve into the complex interplay between the immune system and fetal development, particularly highlighting the detrimental effects of AT1R (Angiotensin II Receptor Type 1) autoantibodies during the critical period of late gestation. AT1R autoantibodies have emerged as a significant factor in various pregnancy complications, elucidating their role in inhibiting the PI3K/AKT signaling pathway, which is vital for fetal hepatic glycogen synthesis. This discovery opens a new avenue of understanding in maternal-fetal medicine, suggesting that these autoantibodies could be a contributing factor in fetal metabolic disorders.
The research presents a detailed analysis of how these autoantibodies interfere with the signaling pathways responsible for glycogen synthesis in the fetal liver. Glycogen plays a crucial role in energy storage and metabolism; deficits in its synthesis can have serious implications for fetal development. Understanding the mechanisms that inhibit glycogen synthesis is pivotal in preventing potential deficiencies that could arise postnatally, impacting the child’s metabolism and growth.
One of the critical signaling pathways affected by AT1R autoantibodies is the PI3K/AKT pathway. This pathway is well known for its role in cell growth, proliferation, and survival, particularly in the context of insulin signaling. Bian et al. provide compelling evidence that the presence of AT1R autoantibodies leads to diminished activation of AKT, which subsequently hampers glycogen synthesis in the fetal liver. This finding suggests that autoantibodies may serve not only as biomarkers for various pregnancy-related issues but also as direct modulators of crucial metabolic processes.
Moreover, the study sheds light on the implications of these findings for pregnant individuals. The presence of AT1R autoantibodies could signal a need for closer monitoring of fetal development and metabolic health. Early identification and intervention could help manage potential risks, leading to better outcomes for both mothers and their children. The research highlights that clinical measures should incorporate regular screenings for AT1R autoantibodies to ensure that affected individuals receive appropriate care.
This investigation is particularly timely, considering the rising incidence of metabolic disorders worldwide. The holistic understanding of how maternal immunological factors influence fetal health could lead to preventive strategies that mitigate the effects of such disorders. The authors aptly call for further research into targeted therapies that can inhibit the detrimental effects of these autoantibodies while promoting healthy signaling pathways in fetal development.
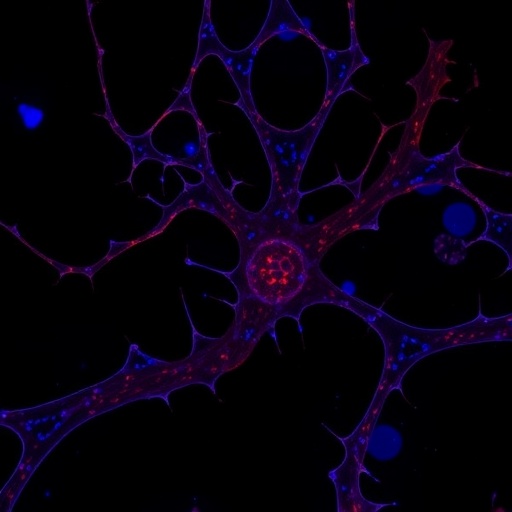
In the study, the researchers utilized a series of sophisticated techniques, including immunofluorescence and Western blot analyses, to elucidate the mechanisms at play. These experimental approaches enabled the team to visualize the cellular interactions and better quantify the impact of AT1R autoantibodies on the PI3K/AKT pathway. Such rigorous methodologies underline the study’s contributions to the field, providing a solid framework upon which additional research can build.
The findings also provoke questions about the origins of these autoantibodies and their implications for maternal health. It is essential to explore whether certain genetic predispositions or environmental factors increase the likelihood of developing AT1R autoantibodies during pregnancy. Understanding these origins could unlock new preventive measures or therapeutic interventions tailored to reduce the prevalence of these autoantibodies in pregnant individuals.
As the medical community digests these findings, the discussion around the significance of the maternal immune system and its impact on fetal growth is set to intensify. With ongoing advancements in maternal-fetal medicine, integrating immunological evaluations alongside traditional prenatal screenings might become standard practice. This comprehensive approach could revolutionize how we monitor and support pregnancies at risk due to immunological factors.
Furthermore, the implications of such research extend beyond the immediate scope of pregnancy. The understanding gleaned from how AT1R autoantibodies influence fetal metabolic processes could open up new perspectives on childhood obesity and metabolic syndrome. These conditions have roots that often trace back to in utero environments, underscoring the need for a preventative framework starting before birth.
In conclusion, the work of Bian and colleagues represents a significant leap in our understanding of the links between immune responses and fetal development. By exploring the molecular pathways impacted by AT1R autoantibodies, this study challenges existing paradigms and invites a re-evaluation of prenatal care practices. The findings underscore the importance of interdisciplinary approaches in tackling complex issues related to maternal and fetal health, demonstrating that robust communication between immunologists, endocrinologists, and obstetricians is essential for advancing care strategies.
As we continue to explore the dynamic relationships underlying pregnancy and fetal development, the research sets the stage for future studies aimed at deciphering the intricate relationship between maternal immunity and fetal metabolic health. Research efforts must persist to ensure that the next generation is equipped for optimal health from the very beginning of life.
This study is an essential contribution to our understanding of pregnancy complications related to maternal autoantibodies and their potential mechanisms of action in the fetal environment. The exploration of the PI3K/AKT signaling pathway highlights important aspects of metabolic regulation during gestation, prompting a critical assessment of how we approach pregnancy monitoring and care.
As the study encourages further investigation, it reminds the scientific community that behind every statistic are real humans—mothers and children—whose lives could be profoundly affected by the findings of this research. The potential for improved health outcomes based on the findings of this study signals an important step toward addressing the complex challenges posed by immune-mediated pregnancy complications.
In a world increasingly aware of the intricate ties between maternal health and child development, the implications of these findings cannot be overstated. By uncovering the biological mechanisms at play, researchers can pave the way for innovative interventions that may one day ensure healthier pregnancies and thriving children.
The journey of inquiry that leads to understanding these complex mechanisms is just beginning, and as we stand on the cusp of potentially transformative health interventions, the insights gained from this study will undoubtedly resonate across the medical community for years to come.
Subject of Research: The effects of AT1R autoantibodies on fetal hepatic glycogen synthesis and the PI3K/AKT signaling pathway during late gestation.
Article Title: AT1R autoantibody impedes fetal hepatic glycogen synthesis by inhibiting PI3K/AKT signaling pathway during late gestation.
Article References:
Bian, J., Wang, W., Wang, P. et al. AT1R autoantibody impedes fetal hepatic glycogen synthesis by inhibiting PI3K/AKT signaling pathway during late gestation. J Transl Med 23, 1121 (2025). https://doi.org/10.1186/s12967-025-07147-1
Image Credits: AI Generated
DOI: 10.1186/s12967-025-07147-1
Keywords: AT1R, autoantibodies, fetal hepatic glycogen synthesis, PI3K/AKT signaling pathway, late gestation, maternal health, fetal development.