In the delicate realm of neonatal care, particularly among preterm infants, the presence of a patent ductus arteriosus (PDA) remains a significant clinical challenge with far-reaching implications. PDA, a persistent opening between the aorta and pulmonary artery that typically closes soon after birth, when left unresolved, can precipitate fluid imbalances, respiratory distress, and systemic complications. The assessment of its hemodynamic significance is therefore paramount to tailoring timely interventions and improving outcomes for these vulnerable patients. Recent research has started to illuminate more precise diagnostic metrics that may surpass the conventional standards established over decades.
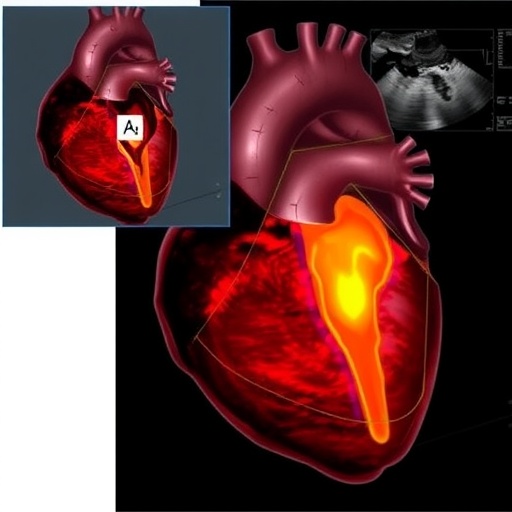
Traditionally, clinicians have relied heavily on the left atrial to aortic root (LA/Ao) ratio—evaluated via echocardiography—as a surrogate marker to determine the hemodynamic impact of PDA. This ratio reflects left atrial enlargement secondary to volume overload, indirectly hinting at the PDA’s physiological burden. However, its accuracy and predictive value have been questioned in neonatal populations, especially those with unstable hemodynamics. The LA/Ao measurement, though routinely employed due to its simplicity, can be influenced by a myriad of factors including artifact, operator dependence, and concurrent cardiac morbidities, potentially diluting its clinical reliability.
A pioneering study spearheaded by Wei, Lin, Chen, and colleagues published in Pediatric Research in 2025 presents compelling evidence that other echocardiographic parameters—specifically the mitral inflow E-wave velocity and left pulmonary artery (LPA) end-diastolic velocity—might offer superior correlation with hemodynamically significant PDA (hsPDA) in preterm infants. These parameters delve more directly into the dynamics of blood flow and cardiac filling pressures, offering a physiologically nuanced perspective that transcends the geometric assumptions inherent in the LA/Ao ratio.
The mitral inflow E-wave velocity reflects the early passive filling phase of the left ventricle during diastole. Elevated E-wave velocities in preterm infants with PDA may indicate amplified left atrial pressures due to increased pulmonary venous return, secondary to left-to-right shunting across the ductus. In this context, the E-wave velocity becomes a non-invasive echo marker that hints at the burden placed on the left heart, serving as a real-time barometer of volume overload and pressure changes engendered by the shunt.
Parallelly, the left pulmonary artery end-diastolic velocity measures the blood flow velocity in the pulmonary artery’s left branch during the relaxation phase of the cardiac cycle. In infants with hsPDA, this velocity surges due to persistently augmented flow across the PDA into the pulmonary circulation, thereby increasing end-diastolic velocity readings. Such a parameter directly quantifies the augmented pulmonary blood flow characteristic of an uncorrected ductus, bypassing the indirect inferences that arise from chamber size assessments like the LA/Ao ratio.
The study meticulously analyzed echocardiographic data from a cohort of preterm infants, juxtaposing these novel measurements against the established LA/Ao ratio and clinically relevant endpoints such as the need for medical or surgical intervention. Their findings revealed a pronounced and statistically significant correlation between elevated mitral inflow E-wave velocities, increased LPA end-diastolic velocities, and the presence of hemodynamically impactful PDA. This relationship eclipsed that of the LA/Ao ratio, suggesting that these flow-derived parameters possess heightened sensitivity and specificity for identifying infants at risk.
These revelations bear profound consequences for clinical practice. The early and precise diagnosis of hsPDA remains critical, as prolonged exposure to pulmonary overcirculation exacerbates morbidities such as bronchopulmonary dysplasia, necrotizing enterocolitis, and intraventricular hemorrhage. By augmenting echocardiographic protocols with these innovative evaluative criteria, neonatologists might refine their decision-making algorithms, opting for earlier intervention or vigilant monitoring tailored to physiological markers rather than anatomical surrogates.
Technological advancements in ultrasound imaging and Doppler flow quantification have enabled the robust acquisition of these velocities with remarkable reproducibility, even in the challenging clinical milieu of small preterm infants. The study underscores the necessity of standardized training and protocol harmonization to ensure these parameters’ consistent application, thus translating research findings into bedside improvements without compromise.
Beyond the immediate clinical ramifications, this research underscores a broader paradigm shift in neonatal cardiology—transitioning from image-based morphometry toward detailed hemodynamic flow analysis. This evolution aligns with a precision medicine ethos that prioritizes individual pathophysiological interrogation over one-size-fits-all criteria. As such, these emerging echocardiographic metrics may pave the path for more granular phenotyping of PDA severity and personalized therapeutic targeting.
Moreover, these insights provoke considerations about longitudinal monitoring strategies. Serial measurement of mitral inflow and LPA velocities could elucidate the temporal trajectory of PDA effects, informing the timing and modality of interventions while minimizing unnecessary treatments. This dynamic, data-driven management framework may mitigate the risks inherent to pharmacological or surgical ductal closure, reducing iatrogenic complications within preterm populations.
While the implications are promising, it is critical to acknowledge ongoing challenges. The integration of these parameters into routine care requires validation across diverse neonatal units, with careful attention to interobserver variability and potential confounders such as concurrent pulmonary hypertension or cardiac anomalies. Prospective multicenter studies would be instrumental in cementing the clinical utility and establishing definitive cutoffs aligned with outcomes.
In addition, the interplay between these velocity measurements and other echocardiographic markers—such as ventricular function indices and pulmonary venous Doppler profiles—warrants exploration. Comprehensive hemodynamic models synthesizing multiple parameters could lead to composite scoring systems, maximizing diagnostic accuracy and predictive power for hsPDA in fragile preterm infants.
The research by Wei and colleagues thus represents a significant leap forward, blending rigorous physiology with advances in echocardiographic technology. Their work challenges entrenched diagnostic paradigms, offering a glimpse of a future where blood flow dynamics are front and center in neonatal cardiologic assessment. Such innovations hold the key to improving survival, reducing morbidity, and ultimately reshaping the narrative of preterm cardiovascular care.
As PDA continues to exact a heavy toll in neonatal intensive care units worldwide, these findings inject fresh hope and direction into clinical practice. By harnessing the subtle yet telling whispers of blood flow patterns within the heart and pulmonary arteries, clinicians can better understand and confront this formidable complication. The fusion of science, technology, and patient-centered precision medicine embodied in this research heralds a new chapter in safeguarding the most vulnerable among us—the tiniest hearts fighting their earliest battles.
Subject of Research: Echocardiographic assessment of hemodynamically significant patent ductus arteriosus (hsPDA) in preterm infants through evaluation of mitral inflow E-wave velocity and left pulmonary artery end-diastolic velocity.
Article Title: Blood flow assessment in echocardiography of hemodynamically significant patent ductus arteriosus in preterm infants.
Article References:
Wei, YJ., Lin, YC., Chen, YJ. et al. Blood flow assessment in echocardiography of hemodynamically significant patent ductus arteriosus in preterm infants. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04449-4
Image Credits: AI Generated