Immunotherapy has revolutionized the landscape of cancer treatment, transforming previously incurable malignancies into potentially manageable diseases by harnessing the patient’s immune system. Despite its monumental promise, a persistent challenge remains: the unpredictable and inconsistent response rates among patients. Addressing this critical issue, researchers at the Cancer Center at Illinois, in collaboration with experts at the National Cancer Institute and MD Anderson Cancer Center, have developed an innovative predictive model designed to forecast the effectiveness of immunotherapy treatments. This model, termed the Liquid Biomarker of Immunotherapy Outcomes (LiBIO) score, is poised to redefine patient stratification and clinical decision-making in cancer immunotherapy.
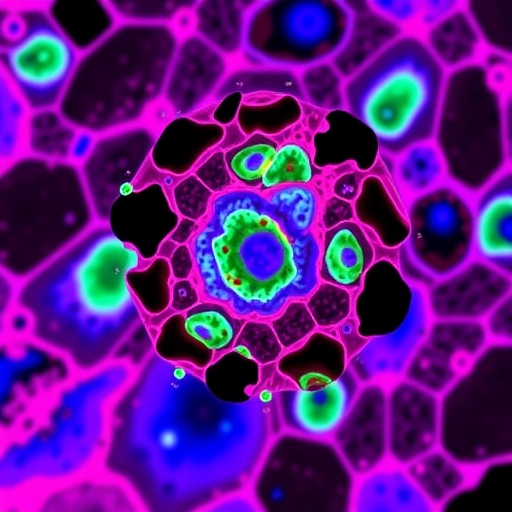
The LiBIO score utilizes a blood-based liquid biopsy technique, a non-invasive approach gaining momentum for its ability to provide dynamic insights into the molecular and immune landscape of cancer patients. The model specifically predicts patient responsiveness to immune checkpoint blockade (ICB) drugs, a class of immunotherapies that have shown remarkable success by unleashing the immune system’s ability to target and destroy tumor cells. By assessing circulating immune cells through serial liquid biopsies, the LiBIO approach offers a real-time window into the evolving cancer-immunity interplay, allowing clinicians to intervene promptly and tailor treatments for optimal outcomes.
Dr. Kun Wang, assistant professor of comparative biosciences and bioengineering, highlights the significance of this advancement. Head and neck squamous cell carcinoma (HNSCC), the focus of this study, often exhibits variable responses to immunotherapy, complicating treatment strategies. “Current clinical practice lacks reliable, minimally invasive biomarkers capable of predicting which patients will derive benefit from ICB therapies,” Wang explains. The LiBIO score fills this critical gap by enabling precise early identification of responders, sparing non-responders from unnecessary treatment-related toxicity and enabling more efficient resource allocation.
Underlying the LiBIO score is a detailed analysis of immune cell populations within peripheral blood samples taken before and after ICB administration. Leveraging a mouse model of HNSCC, the researchers conducted longitudinal monitoring to capture immune dynamics over time. Intriguingly, they identified that an early post-treatment increase in specific subsets of ‘cancer-fighting’ immune cells—namely, effector memory T cells and B cells—correlated strongly with positive therapeutic outcomes. Effector memory T cells are known for their rapid response to tumor antigens, while B cells contribute through antibody production and antigen presentation, suggesting a synergistic immune response to the tumor microenvironment induced by ICB therapy.
The temporal aspect of monitoring was critical in demarcating effective immune activation. Recognizing and validating an optimal early time point post-therapy initiation allowed the scientists to pinpoint a gene expression signature tied to the relevant immune cellular subsets. This gene signature forms the molecular basis of the LiBIO score, serving as a surrogate biomarker that captures the immune system’s readiness to mount an effective anti-tumor attack. This approach contrasts with previous static or invasive tumor biopsies, which fail to dynamically reflect evolving immune responses during treatment.
The predictive accuracy of the LiBIO model surpasses that of existing biomarkers, which often rely on tumor mutational burden or PD-L1 expression levels and yield inconsistent predictive power. Impressively, the LiBIO score demonstrates broad applicability beyond HNSCC, showing promise in predicting immunotherapy responses in malignancies such as breast cancer, lung cancer, and melanoma. This generalizability underscores the pivotal role of systemic immune parameters over tumor-intrinsic factors alone, expanding the clinical utility across diverse cancer types.
The clinical implications of adopting the LiBIO score are profound. By stratifying patients according to their likelihood of benefiting from ICB therapies, clinicians can personalize treatment regimens, reducing exposure to ineffective therapies and associated adverse effects. Moreover, the blood-based nature of this test allows for frequent, minimally invasive monitoring of patients’ immune status during therapy, facilitating dynamic treatment adjustments. Dr. Wang emphasizes, “This tool not only improves therapeutic precision but also empowers clinicians with molecular-level insights during the critical phases of immunotherapy.”
Buoyed by these promising preclinical results, the research team is actively seeking to translate the LiBIO score into clinical trials involving human patients. Dr. Robert Saddawi-Konefka, a key collaborator and physician-scientist at MD Anderson Cancer Center, is spearheading efforts to design and propose trials aimed at validating the biomarker’s predictive power in diverse clinical settings. Although timelines for initiation remain tentative, the groundwork laid by this multi-institutional collaboration instills confidence that human application is imminent.
Future studies will delve deeper into the mechanistic underpinnings of the immune interactions captured by the LiBIO score. While it is established that both effector memory T cells and B cells contribute to enhanced immunotherapy responses, the molecular and cellular crosstalk that potentiates this synergy remains elusive. The research team aims to unravel the precise pathways through which B cells augment T cell-mediated anti-tumor activity. Insights gained may enable the design of next-generation combination immunotherapies that deliberately enhance this interaction to amplify treatment efficacy and overcome resistance.
This pioneering work also raises intriguing questions about the dynamic immune landscape during cancer treatment. The deployment of liquid biopsies to assess immune repertoire diversity—through T cell receptor (TCR) and B cell receptor (BCR) analyses—provides a window into adaptive immune evolution under therapeutic pressure. Understanding how these repertoires shift in responders versus non-responders may identify novel therapeutic targets or resistance mechanisms, heralding a paradigm shift in immunotherapy monitoring.
As the field of cancer immunotherapy advances, tools like the LiBIO score exemplify the fusion of cutting-edge molecular profiling with clinical oncology. By integrating immune biomarkers into treatment algorithms, oncology is moving towards highly personalized interventions that optimize patient outcomes while minimizing unnecessary toxicity. This approach aligns with the broader vision of precision medicine, where dynamic patient-specific data guides not only therapy selection but also real-time adjustments.
In summary, the development of the LiBIO score represents a critical stride in overcoming one of immunotherapy’s major hurdles—the variability in patient response. By exploiting a combination of blood-based immune profiling and longitudinal tracking, this biomarker facilitates early and accurate prediction of treatment success. Its impending clinical translation could revolutionize immunotherapy protocols across multiple cancer types, making treatments safer, more effective, and more accessible. This advancement embodies the promise of translational research to deliver tangible benefits to patients battling cancer worldwide.
Subject of Research:
Immune biomarker development and predictive modeling for immunotherapy response in head and neck squamous cell carcinoma through longitudinal liquid biopsies.
Article Title:
Longitudinal liquid biopsy identifies an early predictive biomarker of immune checkpoint blockade response in head and neck squamous cell carcinoma
News Publication Date:
1-Sep-2025
Web References:
https://www.nature.com/articles/s41467-025-63538-4
References:
Wang, K. et al. Longitudinal liquid biopsy identifies an early predictive biomarker of immune checkpoint blockade response in head and neck squamous cell carcinoma. Nature Communications (2025). DOI: 10.1038/s41467-025-63538-4
Keywords:
Head and neck cancer, immune checkpoint blockade, immunotherapy, liquid biopsy, effector memory T cells, B cells, predictive biomarker, cancer immunotherapy, immune monitoring, precision oncology