In a groundbreaking cohort study analyzing racial disparities within randomized clinical trials (RCTs) for advanced epithelial ovarian cancer, researchers have shed new light on the crucial issue of representation and survival outcomes among diverse patient populations. This comprehensive investigation, involving over 1,900 participants from multiple RCTs, reveals significant underrepresentation of Black and Asian patients relative to their proportions in the broader U.S. population and exposes troubling survival discrepancies that persist despite comparable progression-free survival rates. The findings underscore enduring inequities in clinical trial enrollment and highlight the imperative for equitable inclusion to enable all patient groups to benefit from innovations in oncologic therapeutics.
Ovarian cancer remains one of the most lethal gynecologic malignancies, characterized by late-stage diagnosis and historically poor prognosis. Clinical trials, particularly RCTs, serve as the gold standard for evaluating new treatment modalities and refining therapeutic strategies. Equitable participation across racial and ethnic groups is critical to ensuring that advances in cancer care are broadly applicable and that outcome improvements are shared across the population spectrum. Disparities in trial enrollment, however, jeopardize this goal by limiting the generalizability of findings and potentially perpetuating unequal survival trajectories.
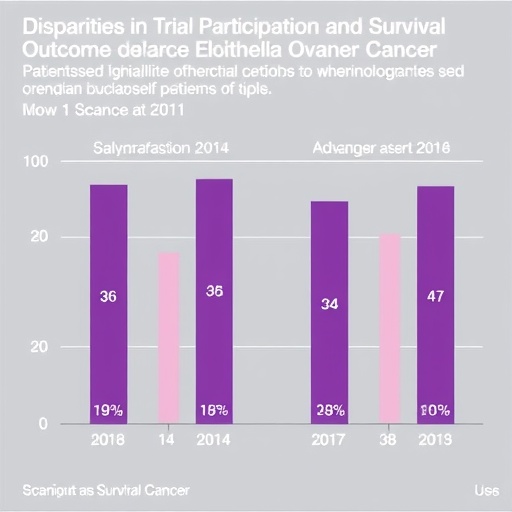
This cohort study meticulously compared trial enrollment demographics to U.S. general population estimates, revealing systemic enrollment imbalances. Black and Asian patients were markedly underrepresented in advanced epithelial ovarian cancer RCTs, despite comprising substantial proportions of the affected population. This underrepresentation suggests a persistent structural failure in clinical trial recruitment efforts and raises concerns about barriers—both systemic and socio-economic—that preclude these populations from accessing cutting-edge investigational therapies.
Interestingly, the survival analyses presented a nuanced picture. Black patients experienced notably poorer overall survival compared to their white and Asian counterparts. Yet, their progression-free survival—the length of time during and after treatment that a patient lives with the disease without it worsening—did not differ significantly from that of other racial groups. This divergence suggests that while initial treatment responses may be comparable, factors influencing long-term survival and disease management might differ substantially, possibly due to disparities in follow-up care, socioeconomic status, comorbid conditions, or access to subsequent lines of therapy.
The mechanisms underlying these survival disparities, despite similar progression-free intervals, warrant detailed exploration. Variables such as treatment adherence, healthcare access, biological differences, and social determinants of health potentially contribute to these observed outcome gaps. Identifying and addressing these heterogeneities is critical for advancing precision oncology and ensuring that survival gains from clinical trial innovations are equitably realized.
Critical to mitigating these disparities is the principle of equitable trial enrollment. Ensuring representative inclusion in clinical research not only validates the external applicability of study findings but also guarantees that all populations benefit from novel diagnostic and therapeutic advances. The study’s findings compel the oncology research community to devise and implement targeted strategies that dismantle enrollment barriers faced by minority populations, including culturally sensitive outreach, logistical support, and policy reforms.
Beyond trial recruitment, efforts must extend to the continuum of cancer care to optimize survival outcomes across racial groups. This includes addressing systemic biases in treatment delivery, enhancing patient education, and improving access to comprehensive supportive and follow-up care. The study unequivocally advocates for a multifaceted approach that marries equitable research participation with equitable clinical management to address entrenched survival disparities.
Importantly, this research contributes to a growing body of evidence highlighting ongoing inequities in healthcare research and outcomes. It exemplifies the urgency of institutional commitment to diversity and inclusion in oncologic clinical trials, reinforcing mandates by regulatory and funding agencies for demographic transparency and representation. Such initiatives are vital to fostering a healthcare environment where clinical evidence serves the entire patient community effectively.
The study’s reliance on data from randomized clinical trials strengthens the robustness of its findings, as randomization minimizes confounding variables, thereby enhancing the validity of the comparison between different racial groups. However, the persistent underrepresentation of minority groups within these trials suggests a paradox where the tool designed to elucidate treatment efficacy across populations itself exhibits demographic biases, a challenge that must be explicitly confronted.
Progression-free survival, a critical endpoint in oncology trials, often serves as a surrogate for treatment efficacy. The study’s observation that progression-free survival rates are similar across racial groups yet overall survival differs signals complex underlying health disparities beyond immediate treatment response. This insight stresses the importance of comprehensive survivorship care and post-progression interventions tailored to address the needs of disadvantaged populations.
The implications of this research transcend ovarian cancer to the broader field of oncology and clinical research. It beckons a reexamination of trial design and recruitment practices to ensure inclusivity, thereby enhancing the scientific rigor and social justice of cancer research. Future studies building on these findings will be critical in developing evidence-based policies and programs to achieve health equity.
In the fight against cancer, the equitable inclusion of diverse patient populations in clinical research is not merely an ethical imperative but a scientific necessity. This study’s revelations about racial disparities in trial participation and survival outcomes highlight the urgent need for ongoing, sustained efforts to transform clinical research and healthcare delivery systems. Only through such concerted actions can we hope to achieve truly equitable cancer care and improve survival outcomes for all patients affected by ovarian cancer.
This pivotal research was spearheaded by Dr. Alex A. Francoeur, whose leadership in oncologic clinical trials has advanced understanding of health disparities in cancer outcomes. The study’s publication in JAMA Network Open ensures open access, enabling researchers, clinicians, and policymakers worldwide to engage with these critical insights.
Subject of Research: Racial disparities in representation and survival outcomes among patients enrolled in randomized clinical trials for advanced epithelial ovarian cancer.
Article Title: Racial Disparities in Clinical Trial Enrollment and Survival Outcomes in Advanced Epithelial Ovarian Cancer
Web References: DOI: 10.1001/jamanetworkopen.2025.38648
Keywords: Ovarian cancer, Clinical trials, Randomization, Population, United States population, Cohort studies, Ethnicity, Medical treatments, Oncology