A groundbreaking study published in BMC Cancer introduces novel insights into the detection of brain metastases (BM) originating from various pathological types of lung cancer using fluorine-18-fibroblast activation protein inhibitor positron emission tomography/computed tomography (^18F-FAPI PET/CT). This pioneering research reveals distinct differences in diagnostic efficacy across lung cancer subtypes, potentially reshaping prognostic evaluation and patient management strategies.
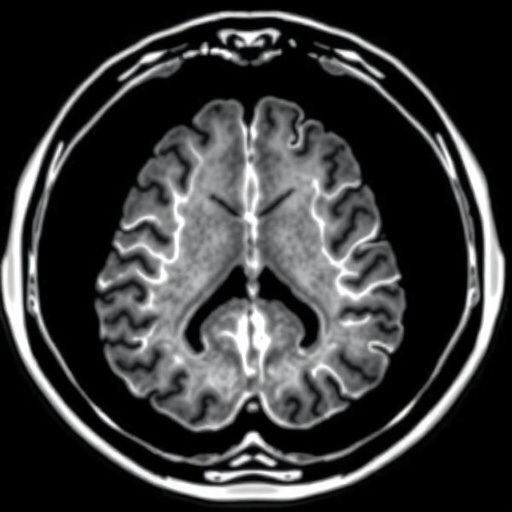
Lung cancer remains one of the deadliest malignancies globally, frequently complicated by the development of brain metastases, which significantly worsen patient outcomes. Traditional imaging methods, particularly craniocerebral magnetic resonance imaging (MRI), are the current standard for detecting BM, offering high sensitivity and detailed anatomical resolution. However, MRI’s ability to characterize metabolic activity or fibroblast activation within lesions is limited, necessitating adjunctive diagnostic tools.
The study prospectively enrolled 18 patients between December 2020 and October 2021, all of whom had histologically confirmed lung cancer and were clinically suspected of harboring brain metastases. Each patient underwent paired imaging with ^18F-FAPI PET/CT and craniocerebral MRI to facilitate a comparative analysis of detection rates. This concurrent imaging strategy enabled precise assessment of ^18F-FAPI PET/CT’s performance relative to the MRI gold standard.
^18F-FAPI PET/CT leverages a radiotracer targeting fibroblast activation protein (FAP), highly expressed in cancer-associated fibroblasts within the tumor microenvironment. This molecular imaging technique exposes the metabolic and stromal components of tumors, which may vary significantly among different cancer histologies. The study measured parameters including maximum and peak standardized uptake values (SUVmax and SUVpeak), alongside tumor-to-background ratios (TBR), to quantify tracer uptake and enhance lesion conspicuity.
Of the 76 BM lesions documented by MRI, only 23 were detected by ^18F-FAPI PET/CT, indicating variability in tracer affinity and imaging sensitivity. Remarkably, adenocarcinoma metastases exhibited the highest detection rate at 48.28%, significantly outperforming large cell carcinoma (16.67%) and small cell carcinoma, for which the detection rate was zero. Squamous carcinoma held an intermediate position with a 35.71% detection rate, not statistically different from adenocarcinoma.
These findings underscore the heterogeneous biological behavior of lung cancer subtypes. The high detection rate in adenocarcinoma may reflect greater fibroblast activation or elevated FAP expression within these lesions, enhancing ^18F-FAPI uptake. Conversely, the lack of detectability in small cell carcinoma suggests either low FAP expression or limited stromal reaction, rendering PET-based fibroblast-targeting ineffective for this subtype.
Statistical analyses demonstrated that squamous carcinoma’s detection rate was significantly superior to that of small cell carcinoma but showed no meaningful difference when compared to large cell carcinoma. Differences between large cell carcinoma and small cell carcinoma also lacked statistical significance. These comparative results highlight the complexity of tumor microenvironments and their impact on molecular imaging performance.
The study’s implications extend beyond diagnostic accuracy; by delineating the differential ^18F-FAPI PET/CT detection rates, clinicians may tailor surveillance and therapeutic interventions more effectively. Enhanced detection of brain metastases in adenocarcinoma patients may facilitate timely interventions, improving prognostication and potentially influencing survival outcomes.
Importantly, the integration of ^18F-FAPI PET/CT with conventional MRI could refine staging and treatment monitoring frameworks. The molecular insights provided by PET imaging complement structural MRI data, offering a dual modality approach that encompasses anatomical and pathophysiological tumor characteristics.
The research also opens avenues for exploring fibroblast activation as a therapeutic target or biomarker in lung cancer brain metastases. Understanding why certain subtypes exhibit robust FAP expression may inform the development of targeted therapies aimed at disrupting the tumor stroma or modifying the metastatic niche within the brain.
Methodologically, the prospective enrollment and paired imaging design enhance the reliability of findings. However, the relatively small sample size and limited number of metastases across subtypes may warrant larger-scale studies to validate these preliminary observations and elucidate underlying mechanisms with greater statistical power.
Future investigations might explore longitudinal imaging to evaluate changes in ^18F-FAPI uptake during treatment or disease progression, shedding light on tumor dynamics and treatment response. Additionally, correlating imaging results with histopathological assessments of FAP expression could deepen understanding of PET tracer specificity and sensitivity.
As the landscape of molecular imaging evolves, ^18F-FAPI PET/CT represents a promising modality for enhancing brain metastasis detection in lung cancer, particularly for adenocarcinoma patients. This technique enriches the diagnostic armamentarium, offering new dimensions in the metabolic and stromal evaluation of metastatic lesions.
Ultimately, this study contributes compelling evidence that varying pathological types of lung cancer differ markedly in their ^18F-FAPI PET/CT detection rates for brain metastases. These insights may herald a shift towards more personalized diagnostic and prognostic strategies, underscoring the critical role of tumor biology in imaging and clinical outcomes.
The research was conducted with institutional review board approval (NO. SDZLEC2021-112-02), affirming adherence to ethical standards. The authors, Li et al., invite further exploration of ^18F-FAPI PET/CT’s utility in broader oncologic contexts, potentially expanding its application in clinical practice.
As molecular imaging technologies advance, the integration of quantitative measures such as SUVmax, SUVpeak, and TBR will become essential to standardize assessments and optimize interpretation across diverse patient populations and tumor types.
In summary, this landmark study elucidates the heterogeneous detection capabilities of ^18F-FAPI PET/CT in brain metastases from lung cancer, with adenocarcinoma showing the highest and small cell carcinoma the lowest detectability. These findings advocate for a nuanced application of molecular imaging tailored to tumor pathology, with significant implications for clinical decision-making and patient management.
Subject of Research: The utility of ^18F-FAPI PET/CT imaging for detecting brain metastases in various pathological types of lung cancer.
Article Title: Different detection rates of brain metastasis in different pathological types of lung cancer by ^18F-FAPI PET/CT.
Article References:
Li, H., Li, P., Zhu, S. et al. Different detection rates of brain metastasis in different pathological types of lung cancer by ^18F-FAPI PET/CT. BMC Cancer 25, 1620 (2025). https://doi.org/10.1186/s12885-025-15078-9
Image Credits: Scienmag.com