In a groundbreaking study encompassing multiple centers, a team of researchers led by Liang, Q., Duan, X., and Yan, H. has unveiled new radiopathomics models that have significant implications for the diagnosis and treatment of adult-type diffuse gliomas. These tumors, which are among the most prevalent and aggressive types of brain cancers, present unique challenges in terms of classification and prognosis. The researchers sought to enhance the predictive capabilities of these models, bridging the gap between imaging and genetic assessments in a comprehensive manner.
The crux of the study lies in the interdisciplinary field of radiopathomics, which combines traditional radiology with advanced machine learning techniques to analyze the intricate patterns evident within imaging data. This melding of disciplines is poised to revolutionize how clinicians approach the management of gliomas. With the advent of sophisticated imaging technologies, it is increasingly possible to extract high-dimensional data that could be pivotal in determining treatment pathways and understanding tumor behavior.
The research began with the collection of a vast pool of imaging and clinical data from multiple institutions, ensuring a diverse and representative sample. The multicenter approach not only enhances the statistical validity of the findings but also allows the models to be trained on a wide array of tumor characteristics. This vast dataset formed the foundation upon which the radiopathomics models were developed, focusing on both molecular subtypes and WHO grading systems. By training the models with this robust data, the researchers aimed to create a predictive tool that is both accurate and reliable.
A significant aspect of this study was the validation process, which is crucial for the credibility of any new therapeutic model. The authors meticulously tested their models against independent datasets, ensuring that the predictions were consistent and reproducible across different populations. This rigorous validation underlines the authors’ commitment to medical rigor and the practical applicability of their findings. Clinicians who deal with gliomas will likely see these models as an invaluable tool in their arsenal, aiding them in making informed decisions.
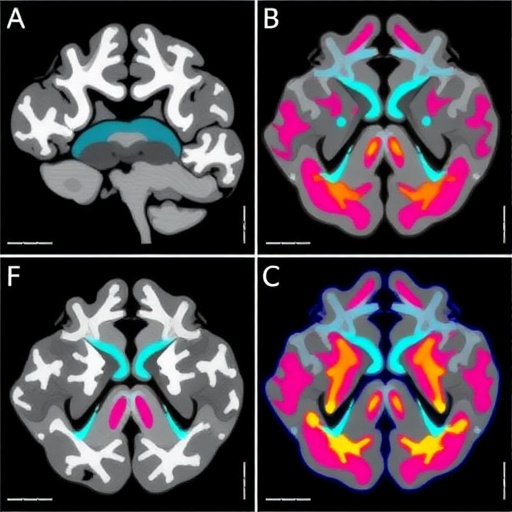
As part of the research methodology, the team utilized advanced imaging techniques such as MRI to gather comprehensive imaging profiles of the gliomas. Using this data, they extracted features that correspond to biological characteristics present within the tumors. These features were then analyzed using state-of-the-art machine learning algorithms capable of discerning patterns that may not be easily noticeable to the human eye. The initiative to harness these insights reflects an innovative approach to brain cancer research that could impact clinical practices significantly.
Another vital aspect of this research is the potential to refine and personalize treatment plans based on the predictions made by the radiopathomics models. For instance, understanding whether a tumor falls into a specific molecular subtype can inform oncologists about the likely responsiveness to particular therapies. This stratified approach represents a shift from the traditional one-size-fits-all strategy, enabling a more targeted and effective treatment pathway.
The implications of developing such predictive models extend beyond mere classification; they may ultimately influence patient outcomes. By accurately predicting the WHO grades of gliomas based on pre-operative imaging, the research team has provided a potential roadmap for anticipatory care. For instance, a better understanding of a tumor’s aggressiveness could lead to earlier intervention and tailored treatment, which is critical in managing gliomas effectively.
Furthermore, the study encourages further exploration into integrating genetic data with imaging profiles. This dual approach could unlock new layers of understanding regarding the molecular mechanisms underpinning tumor behavior. The interplay between genetic mutations and imaging features could reveal patterns that enhance prognostic capabilities even further, heightening our overall comprehension of gliomagenesis.
This research is not just an academic exercise; its real-world applicability positions it at the forefront of neuro-oncological advancements. As glioma treatment continues to evolve, tools like those developed in this study promise to usher in a new era of personalized medicine. The ultimate goal is to harmonize the clinical pathways of care with innovative technological advancements, ensuring that every patient benefits from cutting-edge discoveries.
As we delve deeper into the findings, one cannot discount the collaborative nature of this research. Multicenter studies harness a wealth of expertise and resources, and the collaborative spirit exhibited by these institutions enhances the overall quality and depth of the research. By pooling resources and knowledge, the team has fostered a culture of shared innovation, critical for addressing complex medical challenges like gliomas.
In the realm of brain cancer research, interdisciplinary collaboration emerges as a pivotal force driving advancements. The success of this study exemplifies how the convergence of radiology, pathology, and machine learning can spearhead novel approaches that change the landscape of patient care. As such, findings from this research could serve as a blueprint for future studies aiming to tackle multifaceted medical conditions.
Looking forward, the vision extends beyond gliomas. The advancements in radiopathomics could be extrapolated to other cancer types, highlighting the versatility and potential of this innovative field. Adapting these models for breast cancer, lung cancer, or even less common types could significantly enhance our understanding of cancer heterogeneity and therapy responsiveness, effectively turbocharging the field of oncology.
In conclusion, the development and validation of radiopathomics models by this team stands as a remarkable achievement not only in the realm of glioma research but also within the broader context of medical science. Their innovative approach has the potential to transform how gliomas are diagnosed and treated, ultimately leading to improved patient outcomes. As the findings settle into the existing scientific and clinical frameworks, we may be on the cusp of a new standard in neuro-oncology that champions precision, insight, and collaborative research.
The intricacies of this study point towards a future ripe with potential and innovation. Continued exploration, validation, and application of these models will undoubtedly pave the way for more personalized and effective treatment strategies for all forms of cancer. The journey of integrating machine learning with clinical practice has only just begun, and the implications for patients and healthcare providers alike are nothing short of exhilarating.
Subject of Research: Radiopathomics models for predicting molecular subtypes and WHO grades in adult-type diffuse gliomas.
Article Title: Development and validation of radiopathomics models for predicting molecular subtypes and WHO grades in adult-type diffuse gliomas: a multicenter study.
Article References:
Liang, Q., Duan, X., Yan, H. et al. Development and validation of radiopathomics models for predicting molecular subtypes and WHO grades in adult-type diffuse gliomas: a multicenter study.
J Transl Med 23, 1120 (2025). https://doi.org/10.1186/s12967-025-07073-2
Image Credits: AI Generated
DOI: 10.1186/s12967-025-07073-2
Keywords: radiopathomics, gliomas, predictive models, machine learning, neuro-oncology, personalized treatment.