In a groundbreaking study poised to reshape the landscape of leukemia treatment, researchers from Rutgers Health, collaborating with international partners, have unveiled a molecular mechanism that underlies therapy resistance in acute myeloid leukemia (AML). Despite remarkable advances in oncology, AML remains a formidable adversary, largely due to the eventual failure of frontline therapeutics like venetoclax (Venclexta). This research not only identifies a key protein responsible for this therapeutic evasion but also introduces a promising strategy to counteract it, rekindling hope for improved patient outcomes.
Venetoclax, a highly potent BCL-2 inhibitor, has transformed AML treatment paradigms by inducing apoptosis, or programmed cell death, in malignant cells. While many patients initially respond favorably, resistance almost invariably emerges, dramatically curtailing remission duration and survival rates. The persistence of AML despite such targeted interventions has baffled clinicians and researchers for years, prompting an intensive search for the biological underpinnings of this resistance.
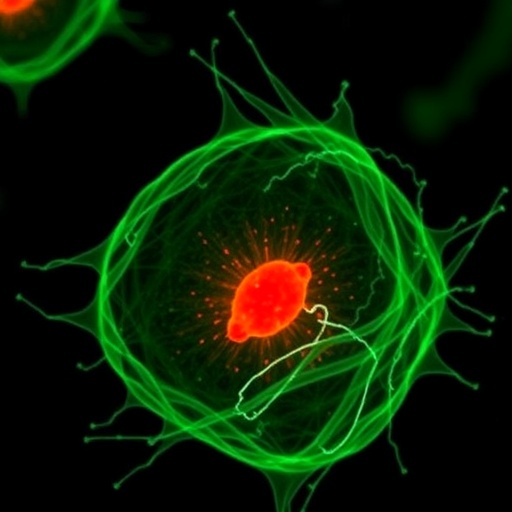
The Rutgers-led team focused on the mitochondria, the powerhouse and apoptotic orchestrator of the cell, to uncover how AML cells dodge venetoclax-induced cell death. Using advanced electron microscopy combined with sophisticated genetic screening techniques, the investigators homed in on a mitochondrial protein called OPA1, a dynamin-like GTPase that tightly regulates mitochondrial inner membrane structure, particularly the morphology of cristae. These cristae folds play a vital role in controlling the release of cytochrome c, a pro-apoptotic factor critical for initiating the cell suicide cascade.
Their analysis revealed that AML cells resistant to venetoclax displayed markedly elevated levels of OPA1. This overexpression drives a remodeling of mitochondrial architecture, resulting in tighter and more abundant cristae folds. This morphological adaptation effectively sequesters cytochrome c within the mitochondria, halting its escape into the cytosol and thereby preventing apoptosis. This elegant, previously uncharacterized defense mechanism provides AML cells with a stealthy means to evade the otherwise lethal effects of venetoclax.
Validating these findings, the researchers scrutinized samples from AML patients. Those who experienced relapse after venetoclax therapy exhibited significantly narrower mitochondrial cristae compared to treatment-naïve patients, with the sharpest alterations observed in cells from patients who had received venetoclax specifically. This patient-derived data strongly corroborates the in vitro and animal model discoveries, underscoring the clinical relevance of OPA1-mediated mitochondrial remodeling in therapy resistance.
Harnessing this knowledge, the team turned to novel small-molecule inhibitors targeting OPA1. Two experimental compounds, developed by collaborators at the University of Padua, were employed in preclinical mouse models engrafted with human AML cells. When these inhibitors were administered in combination with venetoclax, survival times soared, more than doubling relative to animals treated solely with venetoclax. This combination therapy effectively dismantled the mitochondrial defense, restoring apoptotic pathways and eradicating resistant leukemia cells.
Intriguingly, the efficacy of OPA1 inhibition was observed across diverse AML subtypes, including those harboring p53 mutations—a genetic hallmark often linked to poor prognosis and refractory disease. This broad applicability bodes well for clinical translation, as p53-mutant leukemias represent a substantial proportion of resistant cases with limited therapeutic options.
Beyond simply reinstating apoptosis, OPA1 inhibitors appear to invoke additional lethal stress on AML cells. The absence of functional OPA1 imposes a metabolic vulnerability, with leukemia cells becoming heavily dependent on glutamine metabolism. Moreover, these cells showed increased susceptibility to ferroptosis, a distinct form of regulated cell death characterized by iron-dependent lipid peroxidation. These multifaceted mechanisms suggest that OPA1-targeted therapy might subvert AML survival through converging pathways, enhancing therapeutic potency.
Importantly, safety assessments in murine models indicated that OPA1 inhibition does not adversely affect normal hematopoiesis, a critical consideration for any therapy targeting blood cancers. This selective impact on malignant cells lends optimism to the therapeutic window and potential tolerability in future human trials.
Despite these promising results, the journey from bench to bedside is just beginning. The current OPA1 inhibitors serve as lead compounds requiring substantial refinement, especially concerning pharmacokinetics such as solubility and bioavailability. The investigators anticipate developing third-generation inhibitors that will optimize these drug-like properties, paving the way for early-phase clinical studies in humans.
Senior author Christina Glytsou emphasized the transformative nature of these findings, suggesting that targeting mitochondrial morphology could herald a new frontier in combating AML and perhaps other malignancies. Given that OPA1 overexpression and mitochondrial adaptations have been implicated in resistance across multiple cancers, including breast and lung cancers, this strategy may have broad oncologic implications.
This study exemplifies the evolving appreciation of cancer cell metabolism and organelle dynamics as integral players in therapy response and resistance. By decoding the mitochondrial secrets exploited by cancer cells, the Rutgers team has illuminated innovative avenues for intervention that transcend traditional approaches centered exclusively on genetic mutations or surface antigens.
As the scientific community rallies to validate and extend these insights, OPA1 inhibitors stand out as a beacon of hope to overcome one of the deadliest hematologic malignancies. With every step toward overcoming resistance, the prospect of durable remissions and increased survival in AML moves closer to reality. Rutgers Cancer Institute’s leadership in this research underscores their pivotal role in pioneering transformative cancer therapeutics.
Subject of Research: Animals
Article Title: Small-molecule OPA1 inhibitors reverse mitochondrial adaptations to overcome therapy resistance in acute myeloid leukemia
News Publication Date: 15-Oct-2025
Web References: http://dx.doi.org/10.1126/sciadv.adx8662
References: Glytsou et al., Science Advances, 2025, DOI: 10.1126/sciadv.adx8662
Keywords: Leukemia, Cancer, Mitochondria, OPA1, Venetoclax Resistance, Acute Myeloid Leukemia, Apoptosis, Mitochondrial Dynamics, Ferroptosis, Glutamine Metabolism