A groundbreaking study by researchers at The University of Texas at Arlington has uncovered compelling links between state welfare policies and the escalating prevalence of arthritis-related joint pain across the United States. This pioneering research delves into the impact of socioeconomic factors, specifically state-level welfare measures such as minimum wage legislation, Medicaid coverage, and educational attainment, on the trajectory of joint pain over a decade-long period. The findings reveal a complex interaction where policy environments critically shape health outcomes in chronic inflammatory conditions like arthritis.
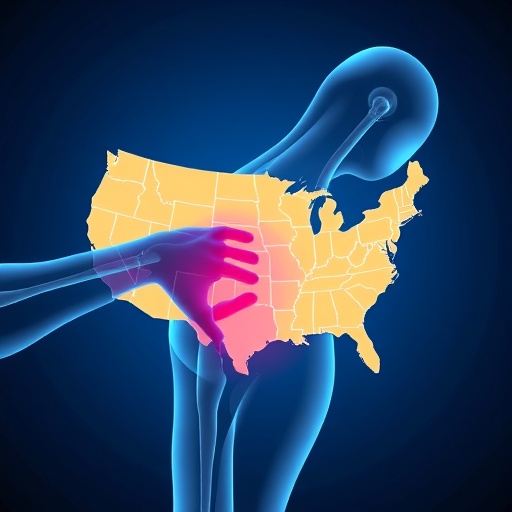
Arthritis, a common and often debilitating immune disorder characterized by joint inflammation and pain, is affecting increasing numbers of Americans. Current estimates from the Centers for Disease Control and Prevention put the figure at approximately 58.5 million, with a notable surge of 4.6 million additional sufferers reporting moderate to severe joint pain between 2011 and 2021. These rising numbers pose urgent questions about the underlying social determinants influencing disease burden, especially in the context of state-level policy variations.
The investigative team, led by Feinuo Sun, an assistant professor of kinesiology at UT Arlington, conducted a detailed longitudinal analysis using data from the Behavioral Risk Factor Surveillance System spanning 2011 to 2021. Unlike prior studies reliant on cross-sectional snapshots, this approach allowed them to examine changes in arthritis pain prevalence over a full decade, providing unprecedented insights into evolving pain trends and their correlations with welfare policies. By deploying fixed effects statistical models, the study controlled for unobserved heterogeneity, isolating the effect of policy differences with greater accuracy.
One of the study’s most striking revelations concerns the geographic variability in joint pain escalation. States like Colorado experienced an extraordinary 26.2% increase in average joint pain prevalence, leading the nation in this adverse trend. Close followers included Hawaii, Nebraska, Kansas, North Dakota, and Texas. Intriguingly, a small cluster of states such as Montana, Wyoming, South Dakota, and New York bucked this trend, exhibiting instead a decline in arthritis-related joint pain over the same timeframe.
Texas presents a particularly interesting case within the context of educational disparities and pain prevalence. Although the state saw a significant overall increase in joint pain, it uniquely experienced a reduction in the educational gap concerning pain. This means that while arthritis pain intensified, the divide between individuals with high and low education levels narrowed. In contrast, states like Colorado witnessed both growing overall pain and a widened educational gap, with the increase disproportionately burdening individuals possessing lower educational attainment.
This nuanced pattern highlights the role of education as a social determinant intertwined with health outcomes and how it interacts with policy frameworks. States where disparities are deepening signal the locations where targeted public health interventions may be most crucial. The findings underscore the necessity of addressing not only clinical care provision but also upstream socioeconomic policies to mitigate chronic pain on a population level.
Central to the study’s conclusions is the influence of Medicaid program generosity in moderating arthritis pain prevalence and educational disparities therein. Medicaid generosity was comprehensively assessed by measuring eligibility thresholds based on income, the inclusion of immigrant populations, the administrative ease of accessing benefits, and the extent of covered services. States that implemented more generous Medicaid policies consistently showed lower joint pain rates and reduced inequalities between educational strata.
This observation points to the critical importance of accessible, comprehensive healthcare coverage in alleviating chronic pain conditions. For adults with lower educational attainment—often correlated with lower income and fewer resources—generous Medicaid programs can bridge the care gap, providing essential medical and rehabilitative services that mitigate the severity and progression of arthritis pain. Policy measures enhancing Medicaid accessibility thus emerge as vital levers to combat health inequities rooted in social stratification.
Furthermore, the study proposes that the mechanism linking welfare policies to arthritis pain extends beyond healthcare access alone; it likely encompasses factors such as stress reduction, improved nutrition, and better occupational conditions facilitated through social support programs. These multidimensional influences collectively affect inflammatory pathways and chronic pain perception, revealing the intricate bi-directional interface between social environment and pathophysiology.
The research team advocates for continued exploration into how individuals’ lived experiences of pain are shaped by evolving policy landscapes. Such insights could enable precision targeting of interventions tailored to state-specific socioeconomic and governance contexts. Additionally, understanding these relationships posits a new paradigm for chronic disease management that integrates public health policy with clinical treatment frameworks.
Overall, this study adds a pivotal voice to ongoing debates about health disparities in the United States, illuminating how diverging state welfare policies directly influence the burden of arthritis-related pain. By linking macro-level governance with micro-level health outcomes, it provides a robust empirical foundation for policymakers seeking to design equity-enhancing health and social programs. In a country markedly stratified by regional welfare strategies, this research highlights the tangible human costs embedded in those policy decisions.
As arthritis continues to impose both individual suffering and economic strain nationwide, these findings signal urgent calls to action. Only through concerted policy reform that expands healthcare coverage, raises educational opportunities, and strengthens social welfare protections can the rising tide of joint pain and associated disparities be stemmed. The study underscores a powerful truth: the path to alleviating chronic pain lies not only in medical innovation but critically in the socio-political determinants that govern wellbeing.
Subject of Research: People
Article Title: Welfare policies, joint pain prevalence and educational gaps in 50 U.S. states from 2011 to 2021: A fixed effects analysis
News Publication Date: 1-Sep-2025
Web References: 10.1016/j.jpain.2025.105539
Keywords: Arthritis, Inflammatory disorders, Pain, Health and medicine